Label: ADDYI- flibanserin tablet, film coated
- NDC Code(s): 58604-214-03, 58604-214-30
- Packager: Sprout Pharmaceuticals, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
Drug Label Information
Updated September 1, 2021
If you are a healthcare professional or from the pharmaceutical industry please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ADDYI safely and effectively.
See full prescribing information for ADDYI.
ADDYI (flibanserin) tablets, for oral use
Initial U.S. Approval: 2015WARNING: HYPOTENSION AND SYNCOPE IN CERTAIN SETTINGS
See full prescribing information for complete boxed warning.
- •
- Use of ADDYI and alcohol together close in time increases the risk of severe hypotension and syncope. Counsel patients to wait at least two hours after consuming one or two standard alcoholic drinks before taking ADDYI at bedtime or to skip their ADDYI dose if they have consumed three or more standard alcoholic drinks that evening. (4, 5.1)
- •
- Severe hypotension and syncope can occur when ADDYI is used with moderate or strong CYP3A4 inhibitors or in patients with hepatic impairment; therefore, ADDYI use in these settings is contraindicated. (4, 5.2, 5.5)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
ADDYI is indicated for the treatment of premenopausal women with acquired, generalized hypoactive sexual desire disorder (HSDD) as characterized by low sexual desire that causes marked distress or interpersonal difficulty and is NOT due to:
- •
- A co-existing medical or psychiatric condition,
- •
- Problems within the relationship, or
- •
- The effects of a medication or other drug substance. (1)
Limitations of Use:
DOSAGE AND ADMINISTRATION
- •
- Recommended dosage is 100 mg taken once daily at bedtime (2.1)
- •
- ADDYI is dosed at bedtime because administration during waking hours increases risks of hypotension, syncope, accidental injury, and central nervous system (CNS) depression (2.1)
- •
- Discontinue treatment after 8 weeks if no improvement (2.3)
DOSAGE FORMS AND STRENGTHS
Tablets: 100 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- •
- Hypotension and Syncope due to an Interaction with Alcohol: After taking ADDYI at bedtime, advise patients to avoid alcohol until the following day. (5.1)
- •
- Hypotension and Syncope with ADDYI Alone: Patients with pre-syncope should immediately lie supine and promptly seek medical help if symptoms do not resolve. (5.4)
- •
- Central Nervous System (CNS) Depression (e.g., Somnolence, Sedation): Can occur with ADDYI alone. Exacerbated by other CNS depressants, and in settings where flibanserin concentrations are increased. Patients should avoid activities requiring full alertness (e.g., operating machinery or driving) until at least six hours after each dose and until they know how ADDYI affects them. (5.3)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥2%) are dizziness, somnolence, nausea, fatigue, insomnia, and dry mouth. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sprout Pharmaceuticals, Inc. at 1-844-746-5745, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- •
- Oral Contraceptives and Other Weak CYP3A4 Inhibitors: Increases flibanserin exposures and incidence of adverse reactions (6.1, 7)
- •
- Strong CYP2C19 Inhibitors: Increases flibanserin exposure which may increase risk of hypotension, syncope, and CNS depression (7)
- •
- CYP3A4 Inducers: Use of ADDYI not recommended; flibanserin concentrations substantially reduced (7)
- •
- Digoxin: Increases digoxin concentrations, which may lead to digoxin toxicity. Increase monitoring of digoxin concentrations (7)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 9/2021
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: HYPOTENSION AND SYNCOPE IN CERTAIN SETTINGS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Missed Dose
2.3 Discontinuation of ADDYI
2.4 Initiation of ADDYI Following Moderate or Strong CYP3A4 Inhibitor Use
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypotension and Syncope due to an Interaction with Alcohol
5.2 Hypotension and Syncope with CYP3A4 Inhibitors
5.3 Central Nervous System Depression
5.4 Hypotension and Syncope with ADDYI Alone
5.5 Syncope and Hypotension in Patients with Hepatic Impairment
5.6 Hypersensitivity Reactions
5.7 Mammary Tumors in Female Mice
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 CYP2C19 Poor Metabolizers
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Studies in Premenopausal HSDD Patients
14.2 Effects on Driving
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: HYPOTENSION AND SYNCOPE IN CERTAIN SETTINGS
Interaction with Alcohol
The use of ADDYI and alcohol together close in time increases the risk of severe hypotension and syncope [see Warnings and Precautions (5.1)]. Counsel patients to wait at least two hours after consuming one or two standard alcoholic drinks before taking ADDYI at bedtime or to skip their ADDYI dose if they have consumed three or more standard alcoholic drinks that evening.
Contraindicated with Strong or Moderate CYP3A4 Inhibitors
The concomitant use of ADDYI and moderate or strong CYP3A4 inhibitors increases flibanserin concentrations, which can cause severe hypotension and syncope [see Warnings and Precautions (5.2)]. Therefore, the use of moderate or strong CYP3A4 inhibitors is contraindicated in patients taking ADDYI [see Contraindications (4)].
Contraindicated in Patients with Hepatic Impairment
The use of ADDYI in patients with hepatic impairment increases flibanserin concentrations, which can cause severe hypotension and syncope [see Warnings and Precautions (5.5)]. Therefore, ADDYI is contraindicated in patients with hepatic impairment [see Contraindications (4)].
-
1 INDICATIONS AND USAGE
ADDYI is indicated for the treatment of premenopausal women with acquired, generalized hypoactive sexual desire disorder (HSDD), as characterized by low sexual desire that causes marked distress or interpersonal difficulty and is NOT due to:
- •
- A co-existing medical or psychiatric condition,
- •
- Problems within the relationship, or
- •
- The effects of a medication or other drug substance.
Acquired HSDD refers to HSDD that develops in a patient who previously had no problems with sexual desire. Generalized HSDD refers to HSDD that occurs regardless of the type of stimulation, situation or partner.
Limitations of Use
- •
- ADDYI is not indicated for the treatment of HSDD in postmenopausal women or in men.
- •
- ADDYI is not indicated to enhance sexual performance.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dosage of ADDYI is 100 mg administered orally once per day at bedtime. ADDYI is dosed at bedtime because administration during waking hours increases the risks of hypotension, syncope, accidental injury, and central nervous system (CNS) depression (such as somnolence and sedation).
2.2 Missed Dose
If a dose of ADDYI is missed at bedtime, instruct the patient to take the next dose at bedtime on the next day. Instruct the patient to not double the next dose.
2.3 Discontinuation of ADDYI
Discontinue ADDYI after 8 weeks if the patient does not report an improvement in her symptoms.
2.4 Initiation of ADDYI Following Moderate or Strong CYP3A4 Inhibitor Use
If initiating ADDYI following moderate or strong CYP3A4 inhibitor use, start ADDYI 2 weeks after the last dose of the CYP3A4 inhibitor.
If initiating a moderate or strong CYP3A4 inhibitor following ADDYI use, start the moderate or strong CYP3A4 inhibitor 2 days after the last dose of ADDYI [see Warnings and Precautions (5.2)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
ADDYI is contraindicated in patients:
- •
- Using concomitant moderate or strong CYP3A4 inhibitors [see Boxed Warning and Warnings and Precautions (5.2)].
- •
- With hepatic impairment [see Boxed Warning and Warnings and Precautions (5.5)].
- •
- With known hypersensitivity to ADDYI or any of its components. Reactions, including anaphylaxis, reactions consistent with angioedema (e.g., swelling of the face, lips, and mouth), pruritus, and urticaria have been reported [see Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypotension and Syncope due to an Interaction with Alcohol
Taking ADDYI within two hours after consuming alcohol increases the risk of severe hypotension and syncope. To reduce this risk, counsel patients to wait at least two hours after drinking one or two standard alcoholic drinks before taking ADDYI at bedtime [see Boxed Warning and Adverse Reactions (6.1)]. Patients who drink three or more standard alcoholic drinks should skip their ADDYI dose that evening. One standard alcoholic drink contains 14 grams of pure alcohol and is equivalent to one 12-ounce regular beer (5% alcohol), 5-ounces wine (12% alcohol), or 1.5 ounces of distilled spirits/shot (40% alcohol).
After taking ADDYI at bedtime, advise patients to not use alcohol until the following day.
5.2 Hypotension and Syncope with CYP3A4 Inhibitors
Moderate or Strong CYP3A4 Inhibitors
The concomitant use of ADDYI with moderate or strong CYP3A4 inhibitors significantly increases flibanserin concentrations, which can lead to hypotension and syncope [see Adverse Reactions (6.1)]. The concomitant use of ADDYI with a moderate or strong CYP3A4 inhibitor is contraindicated. If the patient requires a moderate or strong CYP3A4 inhibitor, discontinue ADDYI at least 2 days prior to starting the moderate or strong CYP3A4 inhibitor. In cases where the benefit of initiating a moderate or strong CYP3A4 inhibitor within 2 days of stopping ADDYI clearly outweighs the risk of flibanserin exposure related hypotension and syncope, monitor the patient for signs of hypotension and syncope. Discontinue the moderate or strong CYP3A4 inhibitor for 2 weeks before restarting ADDYI [see Drug Interactions (7)].
Multiple Concomitant Weak CYP3A4 Inhibitors
Concomitant use of multiple weak CYP3A4 inhibitors that may include herbal supplements (e.g., ginkgo, resveratrol) or non-prescription drugs (e.g., cimetidine) could also lead to clinically relevant increases in flibanserin concentrations that may increase the risk of hypotension and syncope [see Drug Interactions (7)].5.3 Central Nervous System Depression
ADDYI can cause CNS depression (e.g., somnolence, sedation). In five 24-week, randomized, placebo-controlled, double-blind trials of premenopausal women with HSDD, the incidence of somnolence, sedation or fatigue was 21% and 8% in patients treated with 100 mg ADDYI once daily at bedtime and placebo, respectively [see Adverse Reactions (6.1) and Clinical Studies (14.1)]. The risk of CNS depression is increased if ADDYI is taken during waking hours, or if ADDYI is taken with alcohol or other CNS depressants, or with medications that increase flibanserin concentrations, such as CYP3A4 inhibitors [see Contraindications (4), Warnings and Precautions (5.1, 5.2), Adverse Reactions (6.1), and Drug Interactions (7)].
Patients should not drive or engage in other activities requiring full alertness until at least 6 hours after taking ADDYI and until they know how ADDYI affects them [see Clinical Studies (14.2)].
5.4 Hypotension and Syncope with ADDYI Alone
The use of ADDYI − without other concomitant medications known to cause hypotension or syncope − can cause hypotension and syncope. In five 24-week, randomized, placebo-controlled, double-blind trials of premenopausal women with HSDD, hypotension was reported in 0.2% and <0.1% of ADDYI-treated patients and placebo-treated patients, respectively; syncope was reported in 0.4% and 0.2% of ADDYI- treated patients and placebo-treated patients, respectively. The risk of hypotension and syncope is increased if ADDYI is taken during waking hours or if higher than the recommended dose is taken [see Warnings and Precautions (5.1, 5.3), Adverse Reactions (6.1), Drug Interactions (7), and Use in Specific Populations (8.7)]. Consider the benefits of ADDYI and the risks of hypotension and syncope in patients with pre-existing conditions that predispose to hypotension. Patients who experience pre-syncope should immediately lie supine and promptly seek medical help if the symptoms do not resolve. Prompt medical attention should also be obtained for patients who experience syncope.
5.5 Syncope and Hypotension in Patients with Hepatic Impairment
The use of ADDYI in patients with any degree of hepatic impairment significantly increases flibanserin concentrations, which can lead to hypotension and syncope. Therefore, the use of ADDYI is contraindicated in patients with hepatic impairment [see Contraindications (4), Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
5.6 Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylaxis, reactions consistent with angioedema (e.g., swelling of the face, lips, and mouth), pruritus, and urticaria have been reported with ADDYI. ADDYI is contraindicated in women with known hypersensitivity to ADDYI or any of its components [see Adverse Reactions (6.2)]. Immediately discontinue ADDYI and initiate appropriate treatment if a hypersensitivity reaction occurs.
5.7 Mammary Tumors in Female Mice
In a 2-year carcinogenicity study in mice, there was a statistically significant and dose-related increase in the incidence of malignant mammary tumors in female mice at exposures 3 and 10 times the recommended clinical dose. No such increases were seen in male mice or in male or female rats [see Nonclinical Toxicology (13.1)]. The clinical significance of these findings is unknown.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- •
- Hypotension and syncope [see Warnings and Precautions (5.1, 5.2, 5.4, 5.5)]
- •
- CNS depression [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The approved 100 mg ADDYI dosage at bedtime was administered to 2,997 premenopausal women with acquired, generalized HSDD in clinical trials, of whom 1672 received treatment for at least 6 months, 850 received treatment for at least 12 months, and 88 received treatment for at least 18 months [see Clinical Studies (14)].
Data from Five 24-Week, Randomized, Double-Blind Placebo-Controlled Trials in Premenopausal Women with HSDD
The data presented below are derived from five 24-week randomized, double-blind, placebo-controlled trials in premenopausal women with acquired, generalized HSDD. In these five trials, the frequency and quantity of alcohol use was not recorded. Three of these trials (Studies 1 through 3) also provided efficacy data [see Clinical Studies (14.1)]. One of these trials (Study 5) did not evaluate the 100 mg bedtime dose.In four trials, 100 mg ADDYI at bedtime was administered to 1543 premenopausal women with HSDD, of whom 1060 completed 24 weeks of treatment. The clinical trial population was generally healthy without significant comorbid medical conditions or concomitant medications. The age range was 18-56 years old with a mean age of 36 years old, and 88% were Caucasian and 9% were Black.
Serious adverse reactions were reported in 0.9% and 0.5% of ADDYI-treated patients and placebo-treated patients, respectively.
Adverse Reactions Leading to Discontinuation
The discontinuation rate due to adverse reactions was 13% among patients treated with 100 mg ADDYI at bedtime and 6% among patients treated with placebo. Table 1 displays the most common adverse reactions leading to discontinuation in four trials of premenopausal women with HSDD.Table 1. Adverse Reactions* Leading to Discontinuation in Randomized, Double-blind, Placebo-controlled Trials in Premenopausal Women with HSDD - *
- Adverse reactions leading to discontinuation of ≥1% of patients receiving 100 mg ADDYI at bedtime and at a higher incidence than placebo-treated patients.
Placebo (N=1556)
ADDYI (N=1543)
Dizziness
0.1%
1.7%
Nausea
0.1%
1.2%
Insomnia
0.2%
1.1%
Somnolence
0.3%
1.1%
Anxiety
0.3%
1%
Most Common Adverse Reactions
Table 2 summarizes the most common adverse reactions reported in four trials of premenopausal women with HSDD. This table shows adverse reactions reported in at least 2% of patients treated with ADDYI and at a higher incidence than with placebo [see Warnings and Precautions (5.3)]. The majority of these adverse reactions began within the first 14 days of treatment.Table 2. Common Adverse Reactions* in Randomized, Double-blind, Placebo-controlled Trials in Premenopausal Women with HSDD - *
- Adverse reactions reported in ≥2% of patients receiving 100 mg ADDYI at bedtime and at a higher incidence than placebo-treated patients.
Placebo
(N=1556)ADDYI
(N=1543)Dizziness
2.2%
11.4%
Somnolence
2.9%
11.2%
Nausea
3.9%
10.4%
Fatigue
5.5%
9.2%
Insomnia
2.8%
4.9%
Dry mouth
1.0%
2.4%
Less Common Adverse Reactions
In four trials in premenopausal women with HSDD treated with 100 mg ADDYI at bedtime, less common adverse reactions (reported in ≥1% but <2% of ADDYI-treated patients and at a higher incidence than with placebo) included:- •
- Anxiety (ADDYI 1.8%; placebo 1.0%),
- •
- Constipation (ADDYI 1.6%; placebo 0.4%),
- •
- Abdominal pain (ADDYI 1.5%; placebo 0.9%),
- •
- Metrorrhagia (ADDYI 1.4%; placebo 1.4%),
- •
- Rash (ADDYI 1.3%; placebo 0.8%),
- •
- Sedation (ADDYI 1.3%; placebo 0.2%), and
- •
- Vertigo (ADDYI 1%; placebo 0.3%).
Appendicitis
In the five trials of premenopausal women with HSDD, appendicitis was reported in 6/3973 (0.2%) flibanserin-treated patients, while there were no reports of appendicitis in the 1905 placebo-treated patients.Accidental Injury
In five trials of premenopausal women with HSDD, accidental injury was reported in 42/1543 (2.7%) ADDYI-treated patients and 47/1905 (2.5%) placebo-treated patients. Among these 89 patients who experienced injuries, 9/42 (21%) ADDYI-treated patients and 3/47 (6%) placebo-treated patients reported adverse reactions consistent with CNS depression (e.g., somnolence, fatigue, or sedation) within the preceding 24 hours.Adverse Reactions in Patients Who Reported Hormonal Contraceptive Use
In four trials of premenopausal women with HSDD, 1466 patients (43%) reported concomitant use of hormonal contraceptives (HC) at study enrollment. These trials were not prospectively designed to assess an interaction between ADDYI and HC. ADDYI-treated patients who reported HC use had a greater incidence of dizziness, somnolence, and fatigue compared to ADDYI-treated patients who did not report HC use (dizziness 9.9% in HC non-users, 13.4% in HC users; somnolence 10.6% in HC non-users, 12.3% in HC users; fatigue 7.5% in HC non-users, 11.4% in HC users). There were no meaningful differences in the incidence of these adverse reactions in placebo-treated patients who reported or did not report HC use [see Drug Interactions (7)].Data from Other Trials
One death occurred in a 54 year-old postmenopausal woman treated with 100 mg ADDYI taken at bedtime (ADDYI is not approved for the treatment of postmenopausal women with HSDD) [see Indications and Usage (1)]. This patient had a history of hypertension and hypercholesterolemia and baseline alcohol consumption of 1-3 drinks daily. She died of acute alcohol intoxication 14 days after starting ADDYI. Blood alcohol concentration on autopsy was 0.289 g/dL. The autopsy report also noted coronary artery disease. A relationship between this patient’s death and use of ADDYI is unknown [see Boxed Warning and Warnings and Precautions (5.1)].Hypotension, Syncope, and CNS Depression in Studies of Healthy Subjects
Hypotension, Syncope, and CNS Depression with Alcohol
Alcohol and ADDYI Administration at the Same Time
The first alcohol interaction study was conducted in 25 healthy subjects (23 men and 2 premenopausal women). The study excluded subjects who drank fewer than five alcoholic drinks per week and those with a history of orthostatic hypotension, or syncope. A single dose of 100 mg ADDYI was administered concurrently with 0.4 g/kg or 0.8 g/kg alcohol in the morning; alcohol was consumed over 10 minutes. Hypotension or syncope requiring therapeutic intervention (ammonia salts and/or placement in supine or Trendelenberg position) occurred in 4 (17%) of the 23 subjects co-administered 100 mg ADDYI and 0.4 g/kg alcohol (equivalent to two 12 ounce cans of beer containing 5% alcohol content, two 5 ounce glasses of wine containing 12% alcohol content, or two 1.5 ounce shots of 80-proof spirit in a 70 kg person). In these four subjects, all of whom were men, the magnitude of the systolic blood pressure reductions ranged from 28 to 54 mmHg and the magnitude of the diastolic blood pressure reductions ranged from 24 to 46 mmHg. In addition, 6 (25%) of the 24 subjects co-administered 100 mg ADDYI and 0.8 g/kg alcohol (equivalent to four 12 ounce cans of beer containing 5% alcohol content, four 5 ounce glasses of wine containing 12% alcohol content, or four 1.5 ounce shots of 80-proof spirit in a 70 kg person) experienced orthostatic hypotension when standing from a sitting position. The magnitude of the systolic blood pressure reduction in these 6 subjects ranged from 22 to 48 mmHg, and the diastolic blood pressure reductions ranged from 0 to 27 mmHg. One of these subjects required therapeutic intervention (ammonia salts and placement supine with the foot of the bed elevated). There were no events requiring therapeutic interventions when ADDYI or alcohol were administered alone.In this study, somnolence was reported in 67%, 74%, and 92% of subjects who received ADDYI alone, ADDYI in combination with 0.4 g/kg alcohol, and ADDYI in combination with 0.8 g/kg alcohol, respectively. [see Boxed Warning, Warnings and Precautions (5.1, 5.3 and 5.4)].
In the second alcohol interaction study, 96 healthy premenopausal women received a single dose of 100 mg ADDYI concurrently with 0.2 g/kg, 0.4 g/kg, or 0.6 g/kg alcohol (equivalent to one, two or three alcoholic drinks in a 70 kg person, respectively) in the morning. The study excluded subjects with a history of syncope, orthostatic hypotension, hypotensive events, and dizziness, and those with a resting systolic blood pressure less than 110 mmHg or diastolic blood pressure less than 60 mmHg.
In this study, no subjects experienced syncope or hypotension requiring therapeutic intervention. However, subjects who were already hypotensive (blood pressure below 90/60 mmHg) or symptomatic (e.g., dizzy) while in the semi-recumbent position were not permitted to stand for orthostatic measurements, and those with blood pressures below 90/40 mmHg while in the semi-recumbent position had blood pressures repeated until it was deemed safe for them to change position. More subjects had missing or delayed orthostatic measurements (in general, due to hypotension or dizziness) when receiving ADDYI and alcohol, compared to those who received alcohol alone or ADDYI alone. This pattern of missing or delayed orthostatic measurements is concerning for a risk of hypotension and syncope if those subjects had been allowed to stand.
In this study, somnolence was reported in 81-89% of subjects administered ADDYI with alcohol, compared to 25-41% of subjects administered alcohol alone and 84% of subjects taking ADDYI alone. Dizziness was reported in 27-40% of subjects administered ADDYI with alcohol, compared to 6-20% of subjects administered alcohol alone and 31% of subjects taking ADDYI alone. [see Warnings and Precautions (5.1, 5.3, 5.4)].
Alcohol Use at Various Time Intervals Before ADDYI Administration
In a third alcohol interaction study, 64 healthy premenopausal women consumed 0.4 g/kg alcohol (equivalent to 2 alcoholic drinks in a 70 kg person) two, four or six hours prior to receiving ADDYI 100 mg or placebo in the afternoon. The study excluded subjects with a history or presence of orthostatic hypotension, history of hypotension, syncope, or dizziness. Prior to receiving alcohol, the subjects in the ADDYI arm had taken ADDYI for three days to achieve steady state. Syncope occurred in one subject who received alcohol alone. The incidences of orthostatic hypotension and hypotension (blood pressure below 90/60 mmHg) at all time points were similar among subjects administered alcohol before ADDYI, subjects administered alcohol alone, and subjects administered ADDYI alone. Three subjects were unable to stand due to feeling dizzy or hypotension; two following alcohol and ADDYI separated by 2 and 6 hours, and one subject who received ADDYI alone.In this study, somnolence was reported in 35-53% of subjects administered ADDYI and alcohol, compared to 5-8% of subjects taking alcohol alone and 50% of subjects taking ADDYI alone. Dizziness was reported in 5-13% of subjects administered ADDYI and alcohol, compared to 0-3% of subjects taking alcohol alone and 12% of subjects taking ADDYI alone.
Alcohol Use in the Evening Before Bedtime ADDYI Administration
In another alcohol interaction study, 24 premenopausal women consumed 0.4 g/kg alcohol (equivalent to 2 alcoholic drinks in a 70 kg person) during the evening meal two and a half to four hours prior to taking ADDYI 100 mg at bedtime. There were no cases of syncope. Upon rising the following morning, the incidence of hypotension was 23% among subjects administered ADDYI after alcohol, 23% among subjects administered alcohol alone and 36% with ADDYI alone. No cases of somnolence or dizziness were reported in this study. Conclusions are limited because blood pressure and orthostatic measurements were not taken after ADDYI administration until the following morning.Hypotension and Syncope with Fluconazole
In a pharmacokinetic drug interaction study of 100 mg ADDYI and 200 mg fluconazole (a moderate CYP3A4 inhibitor, moderate CYP2C9 inhibitor, and a strong CYP2C19 inhibitor) in healthy subjects, hypotension or syncope requiring placement supine with legs elevated occurred in 3/15 (20%) subjects treated with concomitant ADDYI and fluconazole compared to no such adverse reactions in subjects treated with ADDYI alone or fluconazole alone. One of these 3 subjects became unresponsive with a blood pressure of 64/41 mm Hg and required transportation to the hospital emergency department where she required intravenous saline. Due to these adverse reactions, the study was stopped. In this study, the concomitant use of ADDYI and fluconazole increased flibanserin exposure 7-fold [see Warnings and Precautions (5.2), Drug Interactions (7) and Clinical Pharmacology (12.3)].Syncope with Ketoconazole
In a pharmacokinetic drug interaction study of 50 mg flibanserin and 400 mg ketoconazole, a strong CYP3A4 inhibitor, syncope occurred in 1/24 (4%) healthy subjects treated with concomitant flibanserin and ketoconazole, 1/24 (4%) receiving flibanserin alone, and no subjects receiving ketoconazole alone. In this study, the concomitant use of flibanserin and ketoconazole increased flibanserin exposure 4.5-fold [see Warnings and Precautions (5.2), Drug Interactions (7) and Clinical Pharmacology (12.3)].Syncope in Poor CYP2C19 Metabolizers
In a pharmacogenomic study of 100 mg ADDYI in subjects who were poor or extensive CYP2C19 metabolizers, syncope occurred in 1/9 (11%) subjects who were CYP2C19 poor metabolizers (this subject had a 3.2 fold higher flibanserin exposure compared to CYP2C19 extensive metabolizers) compared to no such adverse reactions in subjects who were CYP2C19 extensive metabolizers [see Drug Interactions (7), Use in Specific Populations (8.7) and Clinical Pharmacology (12.5)].6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval of ADDYI. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Immune system disorders: hypersensitivity reactions, including anaphylaxis, reactions consistent with angioedema (e.g., swelling of the face, lips, and mouth), pruritus, and urticaria.
-
7 DRUG INTERACTIONS
Table 3 contains clinically significant drug interactions (DI) with ADDYI.
Table 3: Clinically Significant Drug Interactions with ADDYI Alcohol
Clinical Implications
The coadministration of ADDYI with alcohol increased the risk of hypotension, syncope, and CNS depression compared to the use of ADDYI alone or alcohol alone [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.2)].
Preventing or Managing DI
Counsel patients to wait at least two hours after consuming one or two standard alcoholic drinks before taking ADDYI at bedtime or to skip their ADDYI dose if they have consumed three or more alcoholic drinks that evening. [see Boxed Warning, Warnings and Precautions (5.1), and Adverse Reactions (6.1)].
Other CNS Depressants
Examples
Diphenhydramine, opioids, hypnotics, benzodiazepines
Clinical Implications
The concomitant use of ADDYI with CNS depressants may increase the risk of CNS depression (e.g., somnolence) compared to the use of ADDYI alone.
Preventing or Managing DI
Discuss the concomitant use of other CNS depressants with the patient when prescribing ADDYI.
Moderate or Strong CYP3A4 Inhibitors
Examples of strong CYP3A4 inhibitors
Ketoconazole, itraconazole, posaconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, boceprevir, telaprevir, telithromycin and conivaptan
Examples of moderate CYP3A4 inhibitors
Amprenavir, atazanavir, ciprofloxacin, diltiazem, erythromycin, fluconazole, fosamprenavir, verapamil, and grapefruit juice
Clinical Implications
The concomitant use of ADDYI with moderate or strong CYP3A4 inhibitors increases flibanserin exposure compared to the use of ADDYI alone. The risk of hypotension and syncope is increased with concomitant use of ADDYI and moderate or strong CYP3A4 inhibitors [see Warnings and Precautions (5.2), Adverse Reactions (6.1), and Clinical Pharmacology (12.3)].
Preventing or Managing DI
The concomitant use of ADDYI with moderate or strong CYP3A4 inhibitors is contraindicated.
Weak CYP3A4 Inhibitors
Examples
Oral contraceptives, cimetidine, fluoxetine, ginkgo, ranitidine
Clinical Implications
The concomitant use of ADDYI with multiple weak CYP3A4 inhibitors may increase the risk of adverse reactions.
Preventing or Managing DI
Discuss the use of multiple weak CYP3A4 inhibitors with the patient when prescribing ADDYI.
Strong CYP2C19 Inhibitors
Examples
Proton pump inhibitors, selective serotonin reuptake inhibitors, benzodiazepines, antifungals
Clinical Implications
The concomitant use of ADDYI with strong CYP2C19 inhibitors may increase flibanserin exposure which may increase the risk of hypotension, syncope, and CNS depression.
Preventing or Managing DI
Discuss the use of a strong CYP2C19 inhibitor with the patient when prescribing ADDYI.
CYP3A4 Inducers
Examples
Carbamazepine, phenobarbital, phenytoin, rifabutin, rifampin, rifapetine, St. John's Wort
Clinical Implications
The concomitant use of ADDYI with CYP3A4 inducers substantially decreases flibanserin exposure compared to the use of ADDYI alone.
Preventing or Managing DI
The concomitant use of ADDYI with CYP3A4 inducers is not recommended.
Digoxin or Other P-glycoprotein Substrates
Examples
Digoxin, sirolimus
Clinical Implications
The concomitant use of ADDYI with digoxin, a drug that is transported by P-glycoprotein (P-gp), increases the digoxin concentration [see Clinical Pharmacology (12.3)]. This may lead to digoxin toxicity.
Preventing or Managing DI
Increase monitoring of concentrations of drugs transported by P-gp that have a narrow therapeutic index (e.g., digoxin).
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no studies of ADDYI in pregnant women to inform whether there is a drug-associated risk in humans. In animals, fetal toxicity only occurred in the presence of significant maternal toxicity including reductions in weight gain and sedation. Adverse reproductive and developmental effects consisted of decreased fetal weight, structural anomalies and increases in fetal loss at exposures greater than 15 times exposures achieved with the recommended human dosage [see Data]. Animal studies cannot rule out the potential for fetal harm.In the general population (not taking ADDYI), the estimated background risk of major birth defects is 2% to 4% of live births, and the estimated background risk of miscarriage of clinically recognized pregnancies is 15% to 20%.
Data
Animal Data
Pregnant rats were administered flibanserin at doses of 0, 20, 80 and 400 mg/kg/day (3, 15 and 41 times clinical exposures at the recommended human dose based on AUC) during organogenesis. The highest dose was associated with significant maternal toxicity as evidenced by severe clinical signs and marked reductions in weight gain during dosing. In the litters of high-dose dams, there were decreased fetal weights, decreased ossification of the forelimbs and increased number of lumbar ribs, and two fetuses with anophthalmia secondary to severe maternal toxicity. The no adverse effect level for embryofetal toxicity was 80 mg/kg/day (15 times clinical exposure based on AUC).Pregnant rabbits were administered flibanserin at doses of 0, 20, 40 and 80 mg/kg/day (4, 8 and 16 times the clinical exposure at the recommended human dose) during organogenesis. Marked decreases in maternal body weight gain (>75%), abortion and complete litter resorption were observed at 40 and 80 mg/kg/day indicating significant maternal toxicity at these doses. Increases in resorptions and decreased fetal weights were observed at ≥ 40 mg/kg/day. No treatment-related teratogenic effects were observed in fetuses at any dose level. The no adverse effect level for maternal and embryofetal effects was 20 mg/kg/day (3-4 times clinical exposure based on AUC).
Pregnant rats were administered flibanserin at doses of 0, 20, 80 and 200 mg/kg/day (3, 15 and ~ 20 times clinical exposures at the recommended human dose) from day 6 of pregnancy until day 21 of lactation to assess for effects on peri- and postnatal development. The highest dose was associated with clinical signs of toxicity in pregnant and lactating rats. All doses resulted in sedation and decreases in body weight gain during pregnancy. Flibanserin prolonged gestation in some dams in all dose groups and decreased implantations, number of fetuses and fetal weights at 200 mg/kg/day. Dosing dams with 200 mg/kg also decreased pup weight gain and viability during the lactation period and delayed opening of the vagina and auditory canals. Flibanserin had no effects on learning, reflexes, fertility or reproductive capacity of the F1 generation. The no adverse effect level for maternal toxicity and peri/postnatal effects was 20 mg/kg/day [see Nonclinical Toxicology (13.1)].
8.2 Lactation
Risk Summary
Flibanserin is excreted in rat milk. It is unknown whether flibanserin is present in human milk, whether ADDYI has effects on the breastfed infant, or whether ADDYI affects milk production. Because of the potential for serious adverse reactions including sedation in a breastfed infant, breastfeeding is not recommended during treatment with ADDYI.8.5 Geriatric Use
ADDYI is not indicated for use in geriatric patients. Safety and effectiveness have not been established in geriatric patients.
8.6 Hepatic Impairment
ADDYI is contraindicated for use in patients with any degree of hepatic impairment. Flibanserin exposure increased 4.5-fold in patients with hepatic impairment, compared to those with normal hepatic function, increasing the risk of hypotension, syncope, and CNS depression [see Boxed Warning, Contraindications (4), Warnings and Precautions (5.5), and Clinical Pharmacology (12.3)].
8.7 CYP2C19 Poor Metabolizers
CYP2C19 poor metabolizers had increased flibanserin exposures compared to CYP2C19 extensive metabolizers. Additionally, syncope occurred in a subject who was a CYP2C19 poor metabolizer [see Adverse Reactions (6.1) and Clinical Pharmacology (12.5)]. Therefore, increase monitoring for adverse reactions (e.g., hypotension) in patients who are CYP2C19 poor metabolizers. The frequencies of poor CYP2C19 metabolizers are approximately 2–5% among Caucasians and Africans and approximately 2–15% among Asians.
-
10 OVERDOSAGE
Overdosage of ADDYI may cause an increase in the incidence or severity of any of the reported adverse reactions [see Warnings and Precautions (5.3, 5.4) and Adverse Reactions (6.1)]. In the event of overdosage, treatment should address the symptoms and supportive measures, as needed. There is no known specific antidote for flibanserin.
-
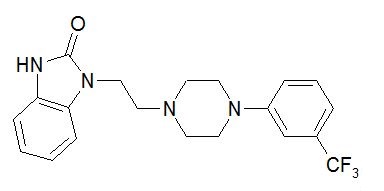
11 DESCRIPTION
ADDYI (flibanserin) is a tablet for oral administration. The chemical name of flibanserin is 2H-Benzimidazol-2-one, 1,3-dihydro-1-[2-[4-[3-(trifluoromethyl)phenyl]-1-piperazinyl]ethyl]. Its empirical formula is C20H21F3N4O and its molecular weight is 390.41.
The structural formula is:
Flibanserin is a white to off-white powder, insoluble in water, sparingly soluble in methanol, ethanol, acetonitrile and toluene, soluble in acetone, freely soluble in chloroform, and very soluble in methylene chloride.
Each ADDYI tablet contains 100 mg of flibanserin. Inactive ingredients consist of lactose monohydrate, microcrystalline cellulose, hypromellose, croscarmellose sodium, magnesium stearate, talc, macrogol, and the coloring agents, titanium dioxide and iron oxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of ADDYI in the treatment of premenopausal women with hypoactive sexual desire disorder is not known.
12.2 Pharmacodynamics
Receptor Binding:
In vitro, flibanserin demonstrated high affinity for the following serotonin (5-hydroxytryptamine or 5-HT) receptors: agonist activity at 5-HT1A and antagonist activity at 5-HT2A. Flibanserin also has moderate antagonist activities at the 5-HT2B, 5-HT2C, and dopamine D4 receptors.Alcohol Interaction
See Clinical Trials Experience (6.1)Cardiac Electrophysiology
The effect of ADDYI on the QT interval was evaluated in a randomized, double-blind, placebo- and active- (single dose moxifloxacin) controlled crossover study in 56 healthy men and women. Subjects in the ADDYI groups received either 50 mg twice a day (equivalent to the daily recommended dosage) or 100 mg three times a day (3 times the daily recommended dosage) administered for 5 days. The time frame for electrocardiogram (ECG) measurements covered maximum plasma concentrations of flibanserin and relevant metabolites. In this study, ADDYI did not prolong the QT interval to any clinically relevant extent. The mean increase in heart rate associated with the 100 mg three times a day dose of ADDYI compared to placebo ranged from 1.7 to 3.2 beats per minute.12.3 Pharmacokinetics
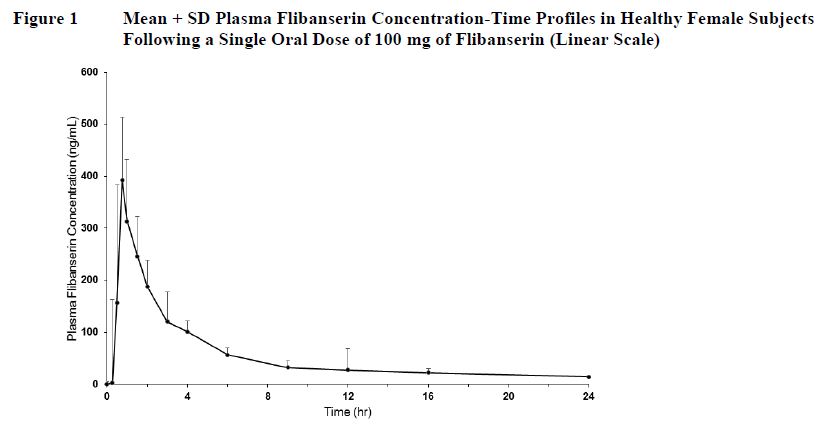
Flibanserin showed dose-proportional pharmacokinetics for Cmax after single oral doses of 100 mg to 250 mg (the recommended and 2.5 times the recommended dosage, respectively) in healthy female subjects. Steady state was achieved after 3 days of dosing. The extent of exposure (AUC0-∞) with once-daily dosing of 100 mg of flibanserin was increased 1.4-fold as compared to a single dose.
Absorption
Following oral administration of a single 100 mg dose of flibanserin in healthy premenopausal women (N=8), mean (SD) Cmax was 419 (206) ng/mL and mean (SD) AUC0-inf was 1543 (511) ng*hr/mL. Median (range) time to reach Cmax was 0.75 (0.75 to 4.0) hours. Absolute bioavailability of flibanserin following oral dosing is 33%.Effect of Food
Food increased the extent of absorption and slowed the rate of absorption of a 50 mg dose of flibanserin (one half the recommended dosage). Low-, moderate-, and high-fat meals increased flibanserin AUC0-inf by 1.18-, 1.43-, and 1.56-fold; increased Cmax by 1.02-, 1.13-, and 1.15-fold; and prolonged median Tmax to 1.5, 0.9, 1.8 hours from 0.8 hours under fasted conditions, respectively.Distribution
Approximately 98% of flibanserin is bound to human serum proteins, mainly to albumin.Elimination
Metabolism
Flibanserin is primarily metabolized by CYP3A4 and, to a lesser extent, by CYP2C19. Based on in vitro and/or in vivo data, CYP1A2, CYP2B6, CYP2C8, CYP2C9, and CYP2D6 contribute minimally to the metabolism of flibanserin. After a single oral solution dose of 50 mg 14C-radiolabeled flibanserin, 44% of the total 14C-flibanserin related radioactivity was recovered in urine, and 51% was recovered in feces. Flibanserin is extensively metabolized to at least 35 metabolites, most of them occurring in low concentrations in plasma. Two metabolites could be characterized that showed plasma concentrations similar to that achieved with flibanserin: 6,21-dihydroxy-flibanserin-6,21-disulfate and 6-hydroxy-flibanserin-6-sulfate. These two metabolites are inactive.Excretion
Flibanserin has a mean terminal half-life of approximately 11 hours.Specific Populations
Hepatic Impairment
Single 50 mg oral doses of flibanserin were administered to 10 patients with mild hepatic impairment (Child-Pugh score of 6 points), 4 patients with moderate hepatic impairment (Child-Pugh score of 8-9 points), and 14 healthy subjects matched by age, weight, and gender. Systemic flibanserin exposure (AUC0-inf) increased 4.5-fold in patients with mild hepatic impairment, compared to subjects with normal hepatic function, and t1/2 was longer (26 hours compared to 10 hours in matching healthy controls). Due to the small number of patients (n=4) with moderate hepatic impairment enrolled in the study, it is not possible to make conclusions about the quantitative effect of moderate hepatic impairment on flibanserin exposure. ADDYI is contraindicated in patients with hepatic impairment [see Warnings and Precautions (5.5)].Renal Impairment
Single 50 mg oral doses of flibanserin were administered to 7 patients with mild to moderate renal impairment (GFR 30 to 80 mL/min), 9 patients with severe renal impairment (GFR <30 mL/min, not on dialysis), and 16 healthy subjects matched by age, weight, and gender. Flibanserin exposure (AUC0-inf) increased 1.1-fold in patients with mild to moderate renal impairment and 1.2-fold in patients with severe renal impairment, compared to the healthy control subjects.Race/Ethnicity
A cross-study comparison between healthy Japanese women and Caucasian women with HSDD showed that flibanserin exposure was approximately 1.4-fold higher in Japanese women. When the mean flibanserin exposure in Japanese women was adjusted for weight, the AUCtau,ss in Japanese women was 2246 ng*hr/mL, which is comparable to 2080 ng*hr/mL in Caucasian women. The similarity in weight-adjusted AUCtau,ss suggests that weight, not race, is the factor contributing to the observed difference in flibanserin exposure between Japanese and Caucasian women.Age
No formal study has been conducted to study the effect of age on flibanserin exposures.Drug Interaction Studies
Drugs that Increase Flibanserin Exposure
The effects of other drugs on the pharmacokinetics of flibanserin are presented in Table 4 as change relative to flibanserin administered alone (test/reference).Moderate CYP3A4/Moderate CYP2C9/Strong CYP2C19 Inhibitor (Fluconazole)
In a study of 15 healthy female subjects, a fluconazole 400 mg loading dose followed by 200 mg administered once daily for 5 days increased flibanserin 100 mg single dose exposure (AUC0-inf) 7-fold and Cmax 2.2-fold compared to flibanserin 100 mg alone. Three of 15 subjects (20%) experienced hypotension or syncope from concomitant use of fluconazole and flibanserin; therefore, the study was stopped early [see Warnings and Precautions (5.2), Adverse Reactions (6.1) and Drug Interactions (7)].Strong CYP3A4 Inhibitor (Ketoconazole)
In a study of 24 healthy female subjects, ketoconazole 400 mg administered once daily for 5 days following a light breakfast increased flibanserin 50 mg single-dose exposure (AUC0-inf) 4.5-fold and Cmax 1.8-fold compared to flibanserin 50 mg alone [see Warnings and Precautions (5.2), Adverse Reactions (6.1) and Drug Interactions (7)].Strong CYP3A4 Inhibitor (Itraconazole)
In a study of 12 healthy male and female subjects, itraconazole 200 mg administered once daily for 4 days following a loading dose of 400 mg increased flibanserin 50 mg single dose exposure (AUC0-inf) 2.6-fold and Cmax 1.7-fold when flibanserin was given 2 hours after itraconazole on Day 5, compared to exposures with flibanserin 50 mg alone. The 200 mg itraconazole dose does not maximally inhibit the CYP3A4 enzyme [see Drug Interactions (7)].Moderate CYP3A4 Inhibitor (Grapefruit Juice)
In a study of 26 healthy female subjects, grapefruit juice (240 mL) increased flibanserin 100 mg single dose exposure (AUC0-inf) by 1.4-fold and Cmax 1.1-fold compared to flibanserin 100 mg alone [see Warnings and Precautions (5.2), Adverse Reactions (6.1) and Drug Interactions (7)].Weak CYP3A4 Inhibitor (Oral Contraceptives)
In a meta-analysis of 17 oral contraceptive users and 91 non-users in Phase 1 studies, the oral contraceptive users had a 1.4-fold higher flibanserin AUC and 1.3‑fold higher Cmax compared to the non-users [see Adverse Reactions (6.1) and Drug Interactions (7)].Strong CYP2D6 Inhibitor (Paroxetine)
Paroxetine is a strong CYP2D6 inhibitor. In a study of 19 healthy male and female subjects, flibanserin exposure decreased by approximately 4% when flibanserin 50 mg twice daily was given with paroxetine compared to flibanserin alone. Paroxetine was dosed at 20 mg once daily for 3 days followed by 40 mg once daily for 7 days.Drugs that Decrease Flibanserin Exposure
Strong CYP3A4 Inducer (Rifampin)
In a study of 24 healthy female subjects, rifampin 600 mg given once daily for 7 days prior to administration of 100 mg flibanserin significantly decreased flibanserin exposure by 95% [see Drug Interactions (7)].
Moderate CYP3A4 Inducer (Etravirine)
Steady state etravirine, a moderate CYP3A4 inducer, decreased flibanserin exposures by approximately 21% [see Drug Interactions (7)].Table 4 Drugs That Increase Flibanserin Exposure - *
- itraconazole dose was not optimal for maximal inhibition of CYP3A4 enzyme.
Coadministered Drug(s) and Dose(s)
Dose of ADDYI
n
Geometric Mean Ratio (90% Confidence Interval) of Pharmacokinetic Parameters of Flibanserin with/without Coadministered Drug
No Effect =1.00Cmax
AUC0-inf
Fluconazole 200 mg
100 mg
15
2.2 (1.8 – 2.8)
7.0 (6.0 – 8.2)
Ketoconazole 400 mg
50 mg
24
1.8 (1.7 – 2.1)
4.5 (4.0 – 5.1)
Itraconazole 200 mg*
50 mg
12
1.7 (1.4 – 2.0)
2.6 (2.1 – 3.0)
Oral Contraceptives
50 mg
39
1.3 (1.1 – 1.6)
1.4 (1.2 – 1.7)
Paroxetine 40 mg
50 mg twice daily
19
1.0 (0.9 – 1.2)
1.0 (0.9 – 1.0)
Effects of Flibanserin on Other Drugs
The effects of flibanserin on the pharmacokinetics of other drugs are presented in Table 5 as change relative to the other drug administered alone (test/reference).Digoxin and P-glycoprotein Substrates
A single center, open-label, randomized, two-way crossover study in 24 healthy men and women evaluated the effect of flibanserin on the pharmacokinetics of digoxin. Flibanserin 100 mg was administered once daily over 5 days followed by a single dose of 0.5 mg digoxin, a P-gp substrate. Flibanserin increased digoxin AUC0-inf by 2.0-fold and Cmax by 1.5-fold, compared to digoxin alone [see Drug Interactions (7)].Drugs Metabolized by CYP3A4 (Simvastatin)
An open-label, randomized, crossover study in 12 healthy men and women evaluated the effect of flibanserin 50 mg twice daily for 4 days on the pharmacokinetics of simvastatin 40 mg once daily. Flibanserin increased the AUC0-inf of simvastatin, a substrate of CYP3A4, 1.3‑fold and Cmax by 1.2-fold. Flibanserin co-administered with simvastatin increased simvastatin acid AUC0-inf by 1.5-fold and Cmax by 1.4-fold.Oral Contraceptives
A study in 24 healthy women evaluated the effect of 100 mg flibanserin once daily for 2 weeks on the pharmacokinetics of a single-dose of ethinyl estradiol (EE) 30 mcg/levonorgestrel (LNG) 150 mcg. Flibanserin increased the EE AUC0-inf by 1.09-fold and the EE Cmax by 1.1-fold. Flibanserin decreased the LNG AUC0-inf by 1.06-fold and did not change the LNG Cmax. [see Adverse Events (6.1), Drug Interactions (7)].Drugs Metabolized by CYP2B6 (Bupropion)
An open-label, randomized, two-period crossover study in 28 healthy women evaluated the effect of flibanserin on the pharmacokinetics of bupropion. Flibanserin 50 mg twice daily was administered for 2 days followed by 100 mg once daily for 13 days. Bupropion 150 mg twice daily was given for 8 days beginning on Day 6 of flibanserin treatment. Flibanserin did not change bupropion AUCt,ss (1.0-fold change) and Cmax (1.0-fold change) but hydroxybupropion AUCt,ss decreased by 9% and Cmax by 11%.Table 5 Effects of Flibanserin on Exposure of Other Drugs Coadministered Drug(s) and Dose(s)
Dose of ADDYI
n
Geometric Mean Ratio (90% Confidence Interval) of Pharmacokinetic Parameters of Coadministered Drug with/without Flibanserin
No Effect =1.00Cmax
AUC0-inf
Simvastatin 40 mg
50 mg twice daily
12
1.7 (1.4 – 2.0)
2.6 (2.1 – 3.1)
Digoxin 0.5 mg
100 mg
24
1.5 (1.3 – 1.6)
2.0 (1.5 – 2.5)
Ethinyl estradiol 30 mcg/
Levonorgestrel 150 mcg100 mg
24
1.1 (1.0 – 1.1)
1.0 (0.9 – 1.0)1.1 (1.0 – 1.2)
1.0 (0.9 – 1.1)Bupropion 150 mg
100 mg
28
1.0 (0.9 – 1.1)
1.0 (1.0 – 1.1)
12.5 Pharmacogenomics
Patients who are poor metabolizers of CYP2D6, CYP2C9 or CYP2C19 are deficient in CYP2D6, CYP2C9 or CYP2C19 enzyme activity, respectively. Extensive metabolizers have normal functioning CYP enzymes.
CYP2C19 Poor Metabolizers
A study comparing flibanserin exposure in CYP2C19 poor metabolizers to CYP2C19 extensive metabolizers was conducted in lieu of a drug interaction study with ADDYI and a strong CYP2C19 inhibitor. In 9 women who were poor metabolizers of CYP2C19, Cmax and AUC0-inf of flibanserin 100 mg once daily increased 1.5-fold (1.1-2.1) and 1.3-fold (0.9-2.1), compared to exposures among 8 extensive metabolizers of CYP2C19. Flibanserin half-life was increased from 11.1 hours in the extensive metabolizers of CYP2C19 to 13.5 hours in the poor metabolizers of CYP2C19 [see Adverse Reactions (6.1) and Use in Specific Populations (8.7)].The frequencies of poor metabolizers of CYP2C19 are approximately 2–5% among Caucasians and Africans and approximately 2–15% among Asians.
CYP2D6 Poor Metabolizers
A study comparing flibanserin exposure in CYP2D6 poor metabolizers to CYP2D6 extensive metabolizers was conducted in addition to a drug interaction study with paroxetine, a strong CYP2D6 inhibitor. In 12 poor metabolizers of CYP2D6, steady state Cmax and AUC of flibanserin 50 mg twice daily was decreased by 4% and increased by 18%, respectively, compared to exposures among 19 extensive metabolizers, intermediate metabolizers and ultra rapid metabolizers of CYP2D6.CYP2C9 Poor Metabolizers
A study comparing flibanserin exposure in CYP2C9 poor metabolizers to CYP2C9 extensive metabolizers was conducted in lieu of a drug interaction study with ADDYI and a strong CYP2C9 inhibitor. In 8 women who were poor metabolizers of CYP2C9, Cmax and AUC0-inf of flibanserin 100 mg once daily decreased 23% and 18%, compared to exposures among 8 extensive metabolizers of CYP2C9. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
A two-year carcinogenicity study was conducted in CD-1 mice with dietary administration of 0, 10, 80, 200 and 1000/1200 mg/kg/day of flibanserin. Statistically significant increases in combined mammary tumors (adenoacanthomas and adenocarcinomas) were observed in female mice administered flibanserin at doses of 200 and 1200 mg/kg/day (exposures, based on AUC, were 3 and 10 times the clinical exposures at the recommended clinical dose). No increases in mammary tumors were observed in male mice. Statistically significant increases were also seen for combined hepatocellular adenomas/carcinomas in female mice treated with flibanserin 1200 mg/kg/day and for hepatocellular carcinomas in male mice treated with flibanserin 1000 mg/kg/day (exposures, based on AUC, were 8 times the clinical exposure at the recommended clinical dose).There were no significant increases in tumor incidence in a two year carcinogenicity study conducted in Wistar rats with dietary administration of 0, 10, 30 and 100 mg/kg/day flibanserin (up to 5-8 times human exposure at the recommended clinical dose).
Mutagenesis
Flibanserin was negative for mutagenesis in vitro in Salmonella typhimurium (Ames test) and in Chinese hamster ovary cells. Flibanserin was positive for chromosomal aberrations in cultured human lymphocytes but negative for chromosomal aberrations in vivo in the rat bone marrow micronucleus assay and negative for DNA damage in rat liver in the Comet assay.Impairment of Fertility
Female and male rats were administered flibanserin 14 and 28 days before mating, respectively, to assess for potential effects on fertility and early reproductive performance. Flibanserin slightly increased the duration of the estrus cycle but had no adverse effects on fertility or early embryonic development at doses up to 200 mg/kg/day (~20 times human exposure at the recommended clinical dose). -
14 CLINICAL STUDIES
14.1 Studies in Premenopausal HSDD Patients
The efficacy of ADDYI for the treatment of HSDD in premenopausal women was established in three 24-week, randomized, double-blind, placebo-controlled trials (Studies 1, 2, and 3). The three trials included premenopausal women with acquired, generalized HSDD of at least 6 months duration. In the clinical trials, acquired HSDD was defined as HSDD that developed in patients who previously had no problems with sexual desire. Generalized HSDD was defined as HSDD that was not limited to certain types of stimulation, situations or partners. The patients were treated with ADDYI 100 mg once daily at bedtime (n = 1187) or placebo (n = 1188). Most of the trial participants were Caucasian (88.6%); the remainder were Black (9.6%) and Asian (1.5%). The mean age of study participants was 36 years old (range 19 to 55 years old); the mean duration in the monogamous, heterosexual relationship was 11 years, and the mean duration of HSDD was approximately 5 years. The completion rate across these three trials was 69% and 78% for the ADDYI and placebo groups, respectively.
These trials each had two co-primary efficacy endpoints, one for satisfying sexual events (SSEs) and the other for sexual desire:
- •
- The change from baseline to Week 24 in the number of monthly SSEs (i.e., sexual intercourse, oral sex, masturbation, or genital stimulation by the partner). The SSEs were based on patient responses to the following questions: “Did you have a sexual event?” and “Was the sex satisfying for you?”
- •
- Studies 1 and 2 had a different sexual desire endpoint than Study 3:
- •
- In Studies 1 and 2, the sexual desire co-primary endpoint was the change from baseline to Week 24 in the calculated monthly sexual desire score and was based on patient responses to the question: “Indicate your most intense level of sexual desire.” Every day, patients rated their sexual desire level from 0 (no desire) to 3 (strong desire) and recorded their response in an electronic Diary (eDiary). These responses were summed over a 28-day period to yield the calculated monthly sexual desire score, which ranged from 0 to 84.
- •
- In Study 3, the desire domain of the Female Sexual Function Index (FSFI Desire) was the sexual desire co-primary endpoint. The desire domain of the FSFI has two questions. The first question asks patients “Over the past 4 weeks, how often did you feel sexual desire or interest?”, with responses ranging from 1 (almost never or never) to 5 (almost always or always). The second question asks patients “Over the past 4 weeks, how would you rate your level (degree) of sexual desire or interest?”, with responses ranging from 1 (very low or none at all) to 5 (very high). The FSFI Desire score was calculated by adding the patient’s responses to these two questions then multiplying that sum by 0.6. The FSFI Desire domain score ranged from 1.2 to 6.
The desire domain of the Female Sexual Function Index (FSFI Desire) was also used as a secondary endpoint in Studies 1 and 2.
The three trials had a secondary endpoint that measured bother (a component of distress) related to sexual desire using Question 13 of the Female Sexual Distress Scale-Revised (FSDS-R). This question asks “How often did you feel: Bothered by low sexual desire?” Patients assessed their sexual distress over a 7-day recall period and responded on a scale of 0 (never) to 4 (always).
The efficacy results from Studies 1, 2, and 3 are summarized in Table 6. In all three trials, ADDYI resulted in statistically significant improvement compared to placebo in the change from baseline in monthly SSEs at Week 24. In Study 1 and 2, there were no statistically significant differences between ADDYI and placebo for the eDiary sexual desire endpoint (change in baseline to Week 24). In contrast, in Study 3 there was statistically significant improvement in the change from baseline to Week 24 in sexual desire (using the FSFI Desire Domain) with ADDYI compared to placebo. The FSFI Desire Domain findings were consistent across all three trials as were the findings for the secondary endpoint that assessed distress using Question 13 of the FSDS-R.
Table 6 Efficacy Results in Premenopausal HSDD Patients in Studies 1, 2, and 3 Study 1 Study 2* Study 3 ADDYI Placebo ADDYI Placebo ADDYI Placebo Full Analysis Set n=280 n=290 n=365 n=372 n=532 n=536 CI = Confidence Interval; NS = not statistically significant; N/A = not applicable
Shaded cells show the results for the co-primary efficacy endpoints for each trial.
e-Diary desire was evaluated as a co-primary endpoint in Studies 1 and 2; FSFI desire was evaluated as a co-primary endpoint in Study 3.
The efficacy results are based on the full analysis set comprised of all randomized patients who took at least one dose of study medication and had at least one on-treatment efficacy assessment. Missing values were imputed using last-observation-carried-forward.
The unadjusted means are presented for the baseline values.
For satisfying sexual events, p-values are based on the Wilcoxon rank sum test stratified by pooled center. Median change from baseline is shown because the data are not normally distributed.
For FSFI-desire, e-Diary desire, and FSDS-R Question 13, reported p-values are based on an ANCOVA model using baseline as a covariate with treatment and pooled center as main effect terms. For the change from baseline, the adjusted least squares mean (standard error) are presented.Number of satisfying sexual events (per 28 days)
Baseline (Mean)
3.0
2.7
2.6
2.7
2.5
2.7
Change from baseline (Mean)
1.6
0.8
1.8
1.1
2.5
1.5
Treatment diff. (95% CI)
0.9 (0.3, 1.4)
0.6 (-0.03, 1.2)
1.0 (0.4, 1.5)
Change from baseline (Median)
1.0
0.0
1.0
0.5
1.0
0.5
Median treatment difference
1.0
0.5
0.5
p-value vs placebo
p<0.01
p<0.01
p<0.0001
e-Diary Desire
Baseline (Mean)
12.9
11.8
12.1
10.2
Not Used
Not Used
Change from baseline at Week 24 (Mean)
9.1
6.9
8.3
6.7
Treatment diff. (95% CI)
2.3 (-0.1, 4.7)
1.7 (-0.5, 4.0)
p-value vs placebo
NS
NS
FSFI Desire
Baseline (Mean)
1.9
1.9
1.8
1.8
1.9
1.9
Change from baseline at Week 24 (Mean)
0.9
0.5
0.9
0.5
1.0
0.7
Treatment diff. (95% CI)
0.4 (0.2, 0.5)
0.3 (0.2, 0.5)
0.3 (0.2, 0.4)
p-value vs placebo
N/A†
N/A†
p<0.0001
FSDS-R Question 13‡
Baseline (Mean)
3.2
3.2
3.2
3.2
3.4
3.4
Change from baseline at Week 24 (Mean)
-0.8
-0.5
-0.8
-0.5
-1.0
-0.7
Treatment diff. (95% CI)
-0.4 (-0.5, -0.2)
-0.3 (-0.4, -0.1)
-0.3 (-0.4, -0.1)
p-value vs placebo
N/A†
N/A†
p=0.0001
Exploratory analyses were conducted to assess whether the treatment effects varied depending on baseline number of SSEs, FSFI desire score, and FSDS-R Question 13 distress score. No notable differences were identified among these subgroups.
Supportive analyses were conducted to help interpret the clinical meaningfulness of the observed treatment effects. These analyses defined responders for each efficacy endpoint by anchoring change from baseline to end of treatment with the Patient's Global Impression of Improvement (PGI‑I). The first analysis considered responders to be those who reported being “much improved” or “very much improved.” In this analysis, the absolute difference in the percentage of responders with ADDYI and the percentage of responders with placebo across the three trials was 8-9% for SSEs (29-39% for ADDYI; 21-31% for placebo), 10-13% for FSFI desire domain (43-48% for ADDYI; 31-38% for placebo), and 7-13% for FSDS-R Question 13 (21-34% for ADDYI; 14-25% for placebo). The second analysis considered responders to be those who reported being at least minimally improved. The absolute difference in the percentage of responders with ADDYI and the percentage of responders with placebo across the three trials was 10-15% for SSEs (44-48% for ADDYI; 33-36% for placebo), 12-13% for FSFI desire domain (43-51% for ADDYI; 31-39% for placebo), and 9-12% for FSDS-R Question 13 (50-60% for ADDYI; 41-48% for placebo).
14.2 Effects on Driving
In a randomized, placebo-controlled, 4-way crossover study in 83 healthy premenopausal female subjects, no adverse effect was detected on measures of driving performance itself or psychomotor performance thought to be important for driving performance when assessed 9 hours following single and multiple doses of ADDYI 100 mg once daily at bedtime or single doses of ADDYI 200 mg at bedtime (two times the maximum recommended dosage) [see Warnings and Precautions (5.3)].
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling (Medication Guide).
Hypotension and Syncope
Inform patients that ADDYI can cause severe hypotension and syncope, particularly when taken close in time with alcoholic drinks or with moderate or strong CYP3A4 inhibitors.
- •
- Counsel patients to wait at least two hours after consuming one or two standard alcoholic drinks before taking ADDYI at bedtime or to skip their ADDYI dose if they have consumed 3 or more standard alcoholic drinks that evening.
After taking ADDYI at bedtime, advise patients to not use alcohol until the following day. - •
- Advise patients that moderate or strong CYP3A4 inhibitors are contraindicated with ADDYI and to ask patients to report the use of a new prescription or non-prescription medication or other products that contain CYP3A4 inhibitors (e.g., grapefruit juice, St. John’s Wort).
- •
- Advise patients who experience pre-syncope or lightheadedness to lie down and to call for help if symptoms persist [see Contraindications (4), Warnings and Precautions (5.1, 5.2)].
CNS Depression
Advise patients that ADDYI can cause CNS depression, such as somnolence and sedation, and that the risk is increased with other CNS depressants and with certain drug interactions (e.g., hypnotics, benzodiazepines, opioids). The risk is also increased if ADDYI is taken during waking hours. Advise patients to avoid engaging in activities requiring full alertness (e.g., operating machinery or driving) until at least 6 hours after the ADDYI dose and until they know how ADDYI affects them [see Warnings and Precautions (5.3)].Nursing Mothers
Advise patients not to breastfeed if they are taking ADDYI [see Use in Specific Populations (8.2)].Bedtime Dosing
Advise patients to take only one tablet at bedtime and not to take ADDYI at any other time of day [see Dosage and Administration (2)].Distributed by:
Sprout Pharmaceuticals, Inc.
Raleigh, NC 27609 USA
Product and trademark licensed from:
Sprout Pharmaceuticals, Inc.Copyright 2019, 2021 Sprout Pharmaceuticals, Inc.
ALL RIGHTS RESERVEDADDYI tablets are covered by U.S. Patents Nos. 7,151,103; 7,420,057; 7,183,410; 8,227,471; 9,468,639; and 9,782,403.
IT5046AJ0909
10005639/01 -
MEDICATION GUIDE
ADDYI®(add-ee)
(flibanserin) TabletsRead this Medication Guide before you start taking ADDYI® and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor.
What is the most important information I should know about ADDYI?
Your risk of severe low blood pressure and fainting (loss of consciousness) is increased if you take ADDYI and:- •
-
drink alcohol close to the time you take your ADDYI dose.
- •
-
Wait at least 2 hours after drinking 1 or 2 standard alcoholic drinks before taking ADDYI at bedtime.
Examples of 1 standard alcoholic drink include:- •
- one 12-ounce regular beer
- •
- 5 ounces of wine
- •
- 1.5 ounces of distilled spirits or shot
- •
- If you drink 3 or more standard alcoholic drinks in the evening, skip your ADDYI dose at bedtime.
- •
- After you have taken your ADDYI at bedtime do not drink alcohol until the following day.
- •
- take certain prescription medicines, over-the-counter medicines, or herbal supplements. Do not take or start taking any prescription medicines, over-the-counter medicines, or herbal supplements while taking ADDYI until you have talked with your doctor. Your doctor will tell you if it is safe to take other medicines or herbal supplements while you are taking ADDYI.
- •
- have liver problems. Do not take ADDYI if you have liver problems.
If you take ADDYI and you feel lightheaded or dizzy, lie down right away. Get emergency medical help or ask someone to get emergency medical help for you if the symptoms do not go away or if you feel like you could faint (lose consciousness). If you faint (lose consciousness), tell your doctor as soon as you can.
What is ADDYI?
ADDYI is a prescription medicine used to treat hypoactive (low) sexual desire disorder (HSDD) in women who have not gone through menopause, who have not had problems with low sexual desire in the past, and who have low sexual desire no matter the type of sexual activity, the situation, or the sexual partner. Women with HSDD have low sexual desire that is troubling to them. Their low sexual desire is not due to:
- •
- a medical or mental health problem
- •
- problems in the relationship
- •
- medicine or other drug use
ADDYI is not for use for the treatment of HSDD in women who have gone through menopause or in men.
ADDYI is not for use to improve sexual performance.
ADDYI is not for use in children.Who should not take ADDYI?
Do not take ADDYI if you:- •
- take certain other medicines. Taking ADDYI with certain other medicines can increase the amount of ADDYI in your blood and cause severe low blood pressure, fainting (loss of consciousness), and sleepiness.
Do not take ADDYI if you are taking any of the following medicines:- •
- certain medicines used to treat HIV-1 infection, such as:
- •
- amprenavir
- •
- atazanavir (REYATAZ®)
- •
- fosamprenavir (LEXIVA)
- •
- ritonavir (NORVIR)
- •
- saquinavir (INVIRASE®)
- •
- nelfinavir (VIRACEPT®)
- •
- indinavir (CRIXIVAN®)
- •
- certain medicines that you take by mouth used to treat fungal infections, such as:
- •
- fluconazole (DIFLUCAN®)
- •
- ketoconazole
- •
- itraconazole (ONMEL, SPORANOX®)
- •
- posaconazole (NOXAFIL®)
- •
- certain antibiotics, including:
- •
- ciprofloxacin (CIPRO, CIPRO XR)
- •
- erythromycin (ERY-TAB®,ERYC®,PCE®)
- •
- telithromycin (KETEK®)
- •
- clarithromycin (BIAXIN®)
- •
- certain medicines used to treat Hepatitis C infection, such as:
- •
- boceprevir (VICTRELIS®)
- •
- telaprevir
- •
- certain medicines used to treat high blood pressure, chest pain (angina), or other heart problems, such as:
- •
- diltiazem (CARDIZEM®,CARDIZEM CD®, CARDIZEM LA®, CARTIA XT, DILT CD, DILTZAC, TAZTIA XT, Tiazac®)
- •
- verapamil (CALAN®, CALAN® SR, COVERA-HS®, Verelan®, Verelan PM)
- •
- conivaptan (Vaprisol®)
- •
- nefazodone: a medicine used to treat depression
Ask your doctor or pharmacist if you are not sure if you take any of the medicines listed above.
These are examples of the medicines that you should not take if you are taking ADDYI. Tell your doctor about all of the medicines you take before you start taking ADDYI.
- •
- have liver problems
What should I tell my doctor before taking ADDYI?
Before you take ADDYI, tell your doctor about all of your medical conditions, including if you:- •
- drink alcohol, use drugs or have a history of alcohol or drug abuse
- •
- have ever had depression or other mental health problems
- •
- have low blood pressure or a medical condition that can cause low blood pressure
- •
- are pregnant or plan to become pregnant. It is not known if ADDYI will harm your unborn baby.
- •
- are breastfeeding or plan to breastfeed. It is not known if ADDYI passes into your breast milk. You and your doctor should decide if you will take ADDYI or breastfeed. You should not do both.
Tell your doctor about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. ADDYI can affect the way other medicines work, and other medicines can affect the way ADDYI works, and can cause serious side effects.
Know the medicines and herbal supplements you take. Keep a list of them to show your doctor or pharmacist each time you get a new medicine.How should I take ADDYI?
- •
- Take ADDYI exactly as your doctor tells you to take it.
- •
- Take 1 ADDYI tablet one time a day at bedtime.
- •
- Take ADDYI only at bedtime. Taking ADDYI at a time other than bedtime can increase your risk of low blood pressure, fainting (loss of consciousness), accidental injury, and sleepiness.
- •
- If you drink alcohol, see "What is the most important information I should know about ADDYI?"
- •
- If you skip a dose of ADDYI, take your next dose at bedtime the next day.
- •
- If you miss a dose of ADDYI, skip your missed dose. Take your next dose at bedtime the next day. Do not take ADDYI the next morning or double your next dose. If you take too much ADDYI, call your doctor.
- •
- Tell your doctor if your symptoms of HSDD have not improved after you have taken ADDYI for 8 weeks.
What should I avoid while taking ADDYI?
- •
- Do not drink alcohol close to the time you take your ADDYI dose because this increases your risk of severe low blood pressure and fainting (loss of consciousness).
- •
- Do not drive, operate machinery, or do things that require clear thinking until at least 6 hours after you take ADDYI and until you know how ADDYI affects you.
- •
- Do not drink grapefruit juice if you take ADDYI. Drinking grapefruit juice during your treatment with ADDYI increases your risk of severe low blood pressure and fainting (loss of consciousness).
- •
- You should not take the herbal supplements St. John’s Wort, ginkgo, or resveratrol or certain over-the-counter medicines such as cimetidine until you talk to your doctor. Taking ADDYI with these herbal supplements and over-the-counter medicine may increase your risk of low blood pressure, fainting (loss of consciousness), and sleepiness.
What are the possible side effects of ADDYI?
ADDYI can cause serious side effects, including:- •
- See “What is the most important information I should know about ADDYI?”
- •
- Sleepiness is a common side effect of ADDYI and can be serious. Taking ADDYI can increase your risk of sleepiness if taken during waking hours, if you drink alcohol, or take certain medicines or herbal supplements.
- •
- Low blood pressure and fainting (loss of consciousness) can happen when you take ADDYI even if you do not drink alcohol or take other medicines or herbal supplements. Your risk of low blood pressure and fainting (loss of consciousness) is increased if ADDYI is taken during waking hours, if you drink alcohol within 2 hours of taking ADDYI, or if you take certain medicines or herbal supplements.
The most common side effects of ADDYI include:
- •
- dizziness
- •
- nausea
- •
- tiredness
- •
- difficulty falling asleep or staying asleep
- •
- dry mouth
These are not all of the possible side effects of ADDYI.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store ADDYI?
- •
- Store ADDYI at room temperature between 68°F to 77°F (20°C to 25°C).
Keep ADDYI and all medicines out of the reach of children.
General information about the safe and effective use of ADDYI
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ADDYI for a condition for which it was not prescribed. Do not give ADDYI to other people, even if they have the same symptoms that you have. It may harm them. You can ask your doctor or pharmacist for information about ADDYI that is written for health professionals.What are the ingredients in ADDYI?
Active ingredient: flibanserin
Inactive ingredients: lactose monohydrate, microcrystalline cellulose, hypromellose, croscarmellose sodium, magnesium stearate, talc, macrogol, and the coloring agents, titanium dioxide and iron oxide.Sprout Pharmaceuticals, Inc. Raleigh, NC 27609 USA
Copyright © 2019 Sprout Pharmaceuticals, Inc.
For more information go to www.ADDYI.com or call 1‑844-PINK-PILL (1-844-746-5745).
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: 10/2019
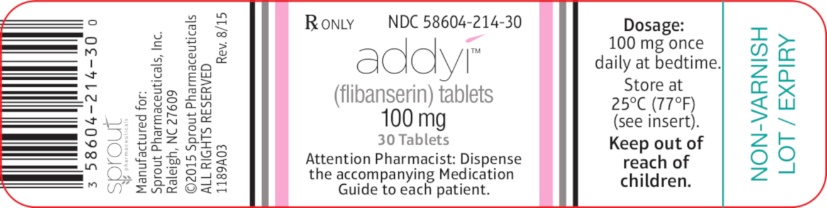
- PRINCIPAL DISPLAY PANEL - Carton Label
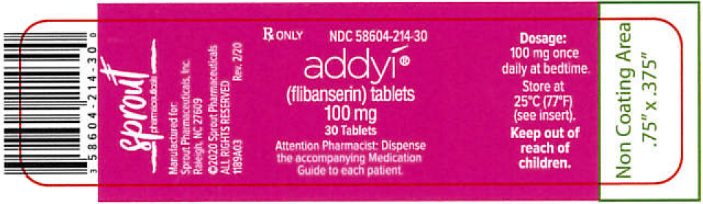
- PRINCIPAL DISPLAY PANEL - Carton Label (New)
- PRINCIPAL DISPLAY PANEL - Bottle Label
- PRINCIPAL DISPLAY PANEL – Bottle Label (New)
-
INGREDIENTS AND APPEARANCE
ADDYI
flibanserin tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:58604-214 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Flibanserin (UNII: 37JK4STR6Z) (Flibanserin - UNII:37JK4STR6Z) Flibanserin 100 mg Inactive Ingredients Ingredient Name Strength Lactose Monohydrate (UNII: EWQ57Q8I5X) Microcrystalline Cellulose (UNII: OP1R32D61U) Hypromellose, Unspecified (UNII: 3NXW29V3WO) Croscarmellose Sodium (UNII: M28OL1HH48) Magnesium Stearate (UNII: 70097M6I30) Talc (UNII: 7SEV7J4R1U) Polyethylene Glycol, Unspecified (UNII: 3WJQ0SDW1A) Titanium Dioxide (UNII: 15FIX9V2JP) Ferric Oxide Red (UNII: 1K09F3G675) Product Characteristics Color PINK Score no score Shape OVAL Size 14mm Flavor Imprint Code f100 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:58604-214-30 1 in 1 CARTON 08/18/2015 1 30 in 1 BOTTLE; Type 0: Not a Combination Product 2 NDC:58604-214-03 1 in 1 CARTON 08/18/2015 06/22/2017 2 30 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022526 08/18/2015 Labeler - Sprout Pharmaceuticals, Inc. (067606232)