Label: ACTOPLUS MET- pioglitazone and metformin hydrochloride tablet, film coated
- NDC Code(s): 64764-158-18, 64764-158-41, 64764-158-60
- Packager: Takeda Pharmaceuticals America, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated June 28, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ACTOPLUS MET safely and effectively. See full prescribing information for ACTOPLUS MET.
ACTOPLUS MET (pioglitazone and metformin hydrochloride) tablets, for oral use
Initial U.S. Approval: 2005WARNING: CONGESTIVE HEART FAILURE and LACTIC ACIDOSIS
See full prescribing information for complete boxed warning.
Congestive Heart Failure
- Thiazolidinediones, including pioglitazone, which is a component of ACTOPLUS MET, cause or exacerbate congestive heart failure in some patients. (5.1)
- After initiation of ACTOPLUS MET, and after dose increases, monitor patients carefully for signs and symptoms of heart failure (e.g., excessive, rapid weight gain, dyspnea, and/or edema). If congestive heart failure develops while taking ACTOPLUS MET, consider discontinuation of ACTOPLUS MET or dosage reduction of pioglitazone in ACTOPLUS MET. (5.1)
- ACTOPLUS MET is not recommended in patients with symptomatic heart failure. (5.1)
- Initiation of ACTOPLUS MET in patients with established New York Heart Association (NYHA) Class III or IV heart failure is contraindicated. (4, 5.1)
Lactic Acidosis
- Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. Symptoms included malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Laboratory abnormalities included elevated blood lactate levels, anion gap acidosis, increased lactate:pyruvate ratio; and metformin plasma levels generally greater than 5 mcg/mL. (5.2)
- Risk factors include renal impairment, concomitant use of certain drugs, age ≥65 years old, radiological studies with contrast, surgery and other procedures, hypoxic states, excessive alcohol intake, and hepatic impairment. Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high-risk groups are provided in the Full Prescribing Information. (5.2)
- If lactic acidosis is suspected, discontinue ACTOPLUS MET and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended. (5.2)
RECENT MAJOR CHANGES
Dosage and Administration
Important Dosage and Administration Information (2.1) 06/2024 Recommended Dosage and Administration (2.2) 06/2024 Recommendations for Use in Patients with Renal Impairment (2.3) 06/2024 Recommendations for Congestive Heart Failure (2.4) 06/2024 Coadministration with Strong CYP2C8 Inhibitors (2.5) 06/2024 INDICATIONS AND USAGE
ACTOPLUS MET is a combination of pioglitazone, a thiazolidinedione agonist of peroxisome proliferator receptor gamma, and metformin hydrochloride (HCl), a biguanide, indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. (1)
Limitations of Use:
Not recommended for treatment of type 1 diabetes or diabetic ketoacidosis. (1)
DOSAGE AND ADMINISTRATION
- Obtain liver tests before initiation. If abnormal, use caution when treating with ACTOPLUS MET, investigate the probable cause, treat (if possible), and follow appropriately. (2.1)
- Take orally with meals to reduce gastrointestinal adverse reactions with metformin (2.10)
- Individualize the starting dose based on the patient’s current regimen and titrate the dosage gradually, as needed after assessing therapeutic response and tolerability. The maximum recommended total daily dosage is pioglitazone 45 mg and metformin 2,550 mg. (2.2)
- Recommended starting dosage in patients with NYHA Class I or Class II congestive heart failure is 15 mg of pioglitazone and 850 mg of metformin HCl orally once daily. (2.4)
- Prior to initiation, assess renal function with estimated glomerular filtration rate (eGFR). (2.2)
- Contraindicated in patients with eGFR below 30 mL/min
- Initiation is not recommended in patients with eGFR between 30 to 45 mL/min
- Assess risk/benefit of continuing ACTOPLUS MET if eGFR falls below 45 mL/min
- Discontinue if eGFR falls below 30 mL/min
- Monitor patients for adverse events related to fluid retention after initiation and dose increases. (2.4)
- ACTOPLUS MET may need to be discontinued at time of, or prior to, iodinated contrast imaging procedures. (2.6)
DOSAGE FORMS AND STRENGTHS
Tablets: 15 mg pioglitazone/850 mg metformin HCl. (3)
CONTRAINDICATIONS
- In patients with established New York Heart Association (NYHA) Class III or IV heart failure at the time of ACTOPLUS MET initiation [see Boxed Warning]. (4)
- In patients with severe renal impairment: (eGFR below 30 mL/min). (4)
- In patients with a history of serious hypersensitivity to pioglitazone, metformin HCl, or any of the excipients in ACTOPLUS MET. (4)
- In patients with acute or chronic metabolic acidosis, including diabetic ketoacidosis. (4)
WARNINGS AND PRECAUTIONS
- Congestive heart failure: Fluid retention may occur and can exacerbate or lead to congestive heart failure. Combination use with insulin and use in congestive heart failure NYHA Class I and II may increase risk. Monitor patients for signs and symptoms. (5.1)
- Edema: Dose-related edema may occur. (5.3)
- Hypoglycemia: Consider a lower dose of insulin or insulin secretagogue to reduce risk of hypoglycemia when used in combination with ACTOPLUS MET. (5.4)
- Hepatic effects: Postmarketing reports of hepatic failure, sometimes fatal. Causality cannot be excluded. If liver injury is detected, promptly interrupt ACTOPLUS MET and assess patient for probable cause, then treat cause if possible, to resolution or stabilization. Do not restart ACTOPLUS MET if liver injury is confirmed and no alternate etiology can be found. (5.5)
- Urinary Bladder Tumors: May increase the risk of bladder cancer. Do not use in patients with active bladder cancer. Use caution when using in patients with a prior history of bladder cancer. (5.6)
- Fractures: Increased incidence in female patients. Apply current standards of care for assessing and maintaining bone health. (5.7)
- Macular edema: Postmarketing reports. Recommend regular eye exams in all patients with diabetes according to current standards of care with prompt evaluation for acute visual changes. (5.8)
- Vitamin B12 deficiency: Metformin may lower vitamin B12 levels. Monitor hematologic parameters annually and vitamin B12 at 2 to 3 year intervals and manage any abnormalities. (5.9)
ADVERSE REACTIONS
Most common adverse reactions (>5%) are upper respiratory tract infection, edema, diarrhea, headache and weight gain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals America, Inc. at 1-877-825-3327 and the ACTOPLUS MET website at: www.actoplusmet.com or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Strong CYP2C8 inhibitors (e.g., gemfibrozil): Limit ACTOPLUS MET dose to 15 mg/850 mg daily. (7.1)
- CYP2C8 inducers (e.g., rifampin) may decrease pioglitazone concentrations. (7.2)
- Carbonic anhydrase inhibitors may increase risk of lactic acidosis. Consider more frequent monitoring. (7.3)
- Drugs that reduce metformin clearance (such as ranolazine, vandetanib, dolutegravir, and cimetidine), may increase the accumulation of metformin. Consider the benefits and risks of concomitant use. (7.4)
- Alcohol: Warn patients against excessive alcohol intake. (7.5)
- Use of insulin secretagogues or insulin use may increase the risk for hypoglycemia and may require dose reduction. (7.6)
- Topiramate may decrease pioglitazone concentrations. (7.8)
USE IN SPECIFIC POPULATIONS
- Females and Males of Reproductive Potential: Advise premenopausal females of the potential for an unintended pregnancy. (8.3)
- Pediatrics: Safety and effectiveness have not been established. (8.4)
- Geriatric Use: Assess renal function more frequently. (8.5)
- Hepatic Impairment: Avoid use in patients with hepatic impairment. (8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CONGESTIVE HEART FAILURE and LACTIC ACIDOSIS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
2.2 Recommended Dosage and Administration
2.3 Recommendations for Use in Patients with Renal Impairment
2.4 Recommendations for Congestive Heart Failure
2.5 Coadministration with Strong CYP2C8 Inhibitors
2.6 Discontinuation for Iodinated Contrast Imaging Procedures
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Congestive Heart Failure
5.2 Lactic Acidosis
5.3 Edema
5.4 Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues
5.5 Hepatic Effects
5.6 Urinary Bladder Tumors
5.7 Fractures
5.8 Macular Edema
5.9 Vitamin B12 Levels
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Strong CYP2C8 Inhibitors
7.2 CYP2C8 Inducers
7.3 Carbonic Anhydrase Inhibitors
7.4 Drugs that Reduce Metformin Clearance
7.5 Alcohol
7.6 Insulin Secretagogues or Insulin
7.7 Drugs Affecting Glycemic Control
7.8 Topiramate
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Patients Who Have Inadequate Glycemic Control with Diet and Exercise Alone
14.2 Patients Previously Treated with Metformin
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CONGESTIVE HEART FAILURE and LACTIC ACIDOSIS
Congestive Heart Failure
- Thiazolidinediones, including pioglitazone, which is a component of ACTOPLUS MET, cause or exacerbate congestive heart failure in some patients [see Warnings and Precautions (5.1)].
- After initiation of ACTOPLUS MET, and after dose increases, monitor patients carefully for signs and symptoms of heart failure (e.g., excessive, rapid weight gain, dyspnea, and/or edema). If congestive heart failure develops while taking ACTOPLUS MET, consider discontinuation of ACTOPLUS MET or dosage reduction of pioglitazone in ACTOPLUS MET [see Warnings and Precautions (5.1)].
- ACTOPLUS MET is not recommended in patients with symptomatic heart failure [see Warnings and Precautions (5.1)].
- Initiation of ACTOPLUS MET in patients with established New York Heart Association (NYHA) Class III or IV heart failure is contraindicated [see Contraindications (4), Warnings and Precautions (5.1)].
Lactic Acidosis
- Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (greater than 5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate:pyruvate ratio; and metformin plasma levels generally greater than 5 mcg/mL [see Warnings and Precautions (5.2)].
- Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (e.g., carbonic anhydrase inhibitors such as topiramate), age 65 years old or greater, having a radiological study with contrast, surgery and other procedures, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, and hepatic impairment.
- Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high-risk groups are provided in the Full Prescribing Information [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.2), Drug Interactions (7), Use in Specific Populations (8.6, 8.7)].
- If metformin-associated lactic acidosis is suspected, immediately discontinue ACTOPLUS MET and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended [see Warnings and Precautions (5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
- Obtain liver tests (serum alanine and aspartate aminotransferases, alkaline phosphatase, and total bilirubin) prior to initiating ACTOPLUS MET [see Warnings and Precautions (5.5)].
- ACTOPLUS MET contains 15 mg of pioglitazone and 850 mg of metformin hydrochloride (HCl) in each tablet.
- Take ACTOPLUS MET with meals to reduce gastrointestinal adverse reactions with metformin [see Adverse Reactions (6.1)].
- If a dose is missed, do not double the next dose.
2.2 Recommended Dosage and Administration
Recommended Starting Dosage Based on Current Regimen
Individualize the starting dosage of ACTOPLUS MET based on the patient's current regimen and the available strength of ACTOPLUS MET (see Table 1).
Table 1: Recommended Starting Dosage Based on the Patient’s Current Regimen Current Regimen Starting Dosage of ACTOPLUS MET (15 mg of pioglitazone and 850 mg of metformin HCl per tablet)* - *
- For dosage recommendations for patients with renal impairment and/or congestive heart failure, see Dosage and Administration (2.3, 2.4)
Not treated with either pioglitazone or metformin HCl One tablet orally once daily Metformin HCl One tablet orally once or twice daily. Select a dosage that is as close as possible to the current dosage of metformin HCl Pioglitazone One tablet orally once daily Pioglitazone and metformin HCl Select a dosage that is as close as possible to the current dosage of pioglitazone and metformin HCl while not exceeding three tablets orally per day. Dosage Titration for Additional Glycemic Control
Titrate the ACTOPLUS MET dosage gradually, as needed, after assessing therapeutic response and tolerability.
ACTOPLUS MET may be increased to a maximum recommended total daily dosage of three tablets per day (45 mg of pioglitazone and 2,550 mg of metformin HCl). Total daily dosages of 2,550 mg of metformin HCl may be taken in divided doses three times a day to reduce gastrointestinal adverse reactions [see Adverse Reactions (6.1)].
2.3 Recommendations for Use in Patients with Renal Impairment
- Assess renal function prior to initiation of ACTOPLUS MET and periodically thereafter [see Use in Specific Populations (8.6)].
- ACTOPLUS MET is contraindicated in patients with an estimated glomerular filtration rate (eGFR) below 30 mL/min.
- Initiation of ACTOPLUS MET in patients with an eGFR between 30 to 45 mL/min is not recommended.
- In patients taking ACTOPLUS MET whose eGFR later falls below 45 mL/min, assess the benefit and risk of continuing therapy.
- Discontinue ACTOPLUS MET if the patient’s eGFR later falls below 30 mL/min [see Contraindications (4), Warnings and Precautions (5.2)].
2.4 Recommendations for Congestive Heart Failure
Starting Dosage in Patients with NYHA Class I or II Congestive Heart Failure
For patients with preexisting NYHA Class I or II congestive heart failure, the recommended starting dosage of ACTOPLUS MET is 15 mg of pioglitazone and 850 mg of metformin [see Boxed Warning and Warnings and Precautions (5.1)].
Monitoring for Fluid Retention and Dosage Modifications for Congestive Heart Failure
After initiation of ACTOPLUS MET or with dosage increase, monitor patients carefully for adverse reactions related to fluid retention as has been seen with pioglitazone (e.g., weight gain, edema and signs and symptoms of congestive heart failure).
If congestive heart failure develops while taking ACTOPLUS MET, consider discontinuation of ACTOPLUS MET or dosage reduction of pioglitazone in ACTOPLUS MET [see Boxed Warning and Warnings and Precautions (5.1)].
2.5 Coadministration with Strong CYP2C8 Inhibitors
The maximum recommended dosage of ACTOPLUS MET is one tablet (15 mg of pioglitazone and 850 mg of metformin HCl) once daily when used in combination with gemfibrozil or other strong CYP2C8 inhibitors [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
2.6 Discontinuation for Iodinated Contrast Imaging Procedures
Discontinue ACTOPLUS MET at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/min; in patients with a history of liver disease, alcoholism, or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure; restart ACTOPLUS MET if renal function is stable [see Warnings and Precautions (5.2)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
ACTOPLUS MET is contraindicated in patients with:
- Established NYHA Class III or IV heart failure at the time of ACTOPLUS MET initiation [see Boxed Warning].
- Severe renal impairment (eGFR below 30 mL/min) [see Warnings and Precautions (5.2)].
- A history of serious hypersensitivity to pioglitazone, metformin HCl, or any of the excipients in ACTOPLUS MET.
- Acute or chronic metabolic acidosis, including diabetic ketoacidosis [see Warnings and Precautions (5.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Congestive Heart Failure
Pioglitazone, like other thiazolidinediones, can cause dose-related fluid retention when used alone or in combination with other antidiabetic medications and is most common when pioglitazone is used in combination with insulin. Fluid retention may lead to or exacerbate congestive heart failure. Observe patients for signs and symptoms of congestive heart failure. If congestive heart failure develops while taking ACTOPLUS MET, consider discontinuation of ACTOPLUS MET or dosage reduction of pioglitazone in ACTOPLUS MET [see Boxed Warning, Contraindications (4), Adverse Reactions (6.1)].
5.2 Lactic Acidosis
Lactic Acidosis
There have been postmarketing cases of metformin-associated lactic acidosis, including fatal cases. These cases had a subtle onset and were accompanied by nonspecific symptoms such as malaise, myalgias, abdominal pain, respiratory distress, or increased somnolence; however, hypothermia, hypotension and resistant bradyarrhythmias have occurred with severe acidosis. Metformin-associated lactic acidosis was characterized by elevated blood lactate concentrations (greater than 5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate:pyruvate ratio, and metformin plasma levels generally greater than 5 mcg/mL. Metformin decreases liver uptake of lactate increasing lactate blood levels which may increase the risk of lactic acidosis, especially in patients at risk.
If metformin-associated lactic acidosis is suspected, general supportive measures should be instituted promptly in a hospital setting, along with immediate discontinuation of ACTOPLUS MET. In ACTOPLUS MET-treated patients with a diagnosis or strong suspicion of lactic acidosis, prompt hemodialysis is recommended to correct the acidosis and remove accumulated metformin (metformin HCl is dialyzable, with a clearance of up to 170 mL/min under good hemodynamic conditions). Hemodialysis has often resulted in reversal of symptoms and recovery.
Educate patients and their families about the symptoms of lactic acidosis and if these symptoms occur instruct them to discontinue ACTOPLUS MET and report these symptoms to their healthcare provider.
For each of the known and possible risk factors for metformin-associated lactic acidosis, recommendations to reduce the risk of and manage metformin-associated lactic acidosis are provided below:
Renal Impairment
The postmarketing metformin-associated lactic acidosis cases primarily occurred in patients with significant renal impairment. The risk of metformin accumulation and metformin-associated lactic acidosis increases with the severity of renal impairment because metformin is substantially excreted by the kidney. Clinical recommendations based upon the patient’s renal function include [see Dosage and Administration (2.3), Clinical Pharmacology (12.3)].
- Before initiating ACTOPLUS MET, obtain an eGFR.
- ACTOPLUS MET is contraindicated in patients with an eGFR less than 30 mL/min. Initiation of ACTOPLUS MET is not recommended in patients with eGFR between 30 to 45 mL/min [see Contraindications (4)].
- Obtain an eGFR at least annually in all patients taking ACTOPLUS MET. In patients at increased risk for the development of renal impairment (e.g., the elderly), renal function should be assessed more frequently.
- In patients taking ACTOPLUS MET whose eGFR later falls below 45 mL/min, assess the benefit and risk of continuing therapy.
Drug Interactions
The concomitant use of ACTOPLUS MET with specific drugs may increase the risk of metformin-associated lactic acidosis: those that impair renal function, result in significant hemodynamic change, interfere with acid-base balance or increase metformin accumulation (e.g., cationic drugs) [see Drug Interactions (7)]. Therefore, consider more frequent monitoring of patients.
Age 65 or Greater
The risk of metformin-associated lactic acidosis increases with the patient’s age because elderly patients have a greater likelihood of having hepatic, renal, or cardiac impairment than younger patients. Assess renal function more frequently in elderly patients [see Use in Specific Populations (8.5)].
Radiological Studies with Contrast
Administration of intravascular iodinated contrast agents in metformin-treated patients has led to an acute decrease in renal function and the occurrence of lactic acidosis. Stop ACTOPLUS MET at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/min; in patients with a history of hepatic impairment, alcoholism, or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure, and restart ACTOPLUS MET if renal function is stable.
Surgery and Other Procedures
Withholding of food and fluids during surgical or other procedures may increase the risk for volume depletion, hypotension and renal impairment. ACTOPLUS MET should be temporarily discontinued while patients have restricted food and fluid intake.
Hypoxic States
Several of the postmarketing cases of metformin-associated lactic acidosis occurred in the setting of acute congestive heart failure (particularly when accompanied by hypoperfusion and hypoxemia). Cardiovascular collapse (shock), acute myocardial infarction, sepsis, and other conditions associated with hypoxemia have been associated with lactic acidosis and may also cause prerenal azotemia. When such events occur, discontinue ACTOPLUS MET.
Excessive Alcohol Intake
Alcohol potentiates the effect of metformin on lactate metabolism and this may increase the risk of metformin-associated lactic acidosis. Warn patients against excessive alcohol intake while receiving ACTOPLUS MET.
Hepatic Impairment
Patients with hepatic impairment have developed with cases of metformin-associated lactic acidosis. This may be due to impaired lactate clearance resulting in higher lactate blood levels. Therefore, avoid use of ACTOPLUS MET in patients with clinical or laboratory evidence of hepatic disease.
5.3 Edema
In controlled clinical trials with pioglitazone, edema was reported more frequently in patients treated with pioglitazone than in placebo-treated patients and is dose related [see Adverse Reactions (6.1)]. In postmarketing experience, reports of new onset or worsening of edema have been received.
ACTOPLUS MET should be used with caution in patients with edema. Because thiazolidinediones, including pioglitazone, can cause fluid retention, which can exacerbate or lead to congestive heart failure, ACTOPLUS MET should be used with caution in patients at risk for congestive heart failure. Patients treated with ACTOPLUS MET should be monitored for signs and symptoms of congestive heart failure [see Boxed Warning, Warnings and Precautions (5.1)].
5.4 Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues
Insulin and insulin secretagogues, such as sulfonylureas, are known to cause hypoglycemia. Therefore, a lower dosage of insulin or insulin secretagogue may be required to minimize the risk of hypoglycemia when used in combination with ACTOPLUS MET [see Drug Interactions (7.6, 7.7)].
5.5 Hepatic Effects
There have been postmarketing reports of fatal and non-fatal hepatic failure in patients taking pioglitazone, although the reports contain insufficient information necessary to establish the probable cause. There has been no evidence of drug-induced hepatotoxicity in the pioglitazone controlled clinical trial database to date [see Adverse Reactions (6.1)].
Patients with type 2 diabetes mellitus may have fatty liver disease or cardiac disease with episodic congestive heart failure, both of which may cause liver test abnormalities, and they may also have other forms of liver disease, many of which can be treated or managed. Therefore, obtaining a liver test panel (serum alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase, and total bilirubin) and assessing the patient is recommended before initiating ACTOPLUS MET therapy. In patients with abnormal liver tests, ACTOPLUS MET should be initiated with caution.
Measure liver tests promptly in patients who report symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice. In this clinical context, if the patient is found to have clinically significant liver enzyme elevations (serum ALT greater than three times the ULN) and if abnormal liver tests persist or worsen, ACTOPLUS MET should be interrupted and investigation done to establish the probable cause. ACTOPLUS MET should not be restarted in these patients without another explanation for the liver test abnormalities.
5.6 Urinary Bladder Tumors
Tumors were observed in the urinary bladder of male rats in the two year carcinogenicity study [see Nonclinical Toxicology (13.1)]. In addition, during the three year PROactive clinical trial, 14 patients out of 2,605 (0.54%) randomized to pioglitazone and 5 out of 2,633 (0.19%) randomized to placebo were diagnosed with bladder cancer. After excluding patients in whom exposure to study drug was less than one year at the time of diagnosis of bladder cancer, there were 6 (0.23%) cases on pioglitazone and 2 (0.08%) cases on placebo. After completion of the trial, a large subset of patients was observed for up to 10 additional years, with little additional exposure to pioglitazone. During the 13 years of both PROactive and observational follow-up, the occurrence of bladder cancer did not differ between patients randomized to pioglitazone or placebo [Hazard Ratio (HR) = 1.00; (95% Confidence Interval (CI) : 0.59, 1.72)].
Findings regarding the risk of bladder cancer in patients exposed to pioglitazone vary among observational studies; some did not find an increased risk of bladder cancer associated with pioglitazone, while others did.
A large prospective10 year observational cohort study conducted in the United States (U.S) found no statistically significant increase in the risk of bladder cancer in diabetic patients ever exposed to pioglitazone, compared to those never exposed to pioglitazone [HR = 1.06; (95% CI: 0.89, 1.26)].
A retrospective cohort study conducted with data from the United Kingdom found a statistically significant association between ever exposure to pioglitazone and bladder cancer [HR = 1.63; (95% CI: 1.22, 2.19)].
Associations between cumulative dose or cumulative duration of exposure to pioglitazone and bladder cancer were not detected in some studies including the 10 year observational study in the U.S., but were in others. Inconsistent findings and limitations inherent in these and other studies preclude conclusive interpretations of the observational data.
Pioglitazone may be associated with an increase in the risk of urinary bladder tumors. There are insufficient data to determine whether pioglitazone is a tumor promoter for urinary bladder tumors.
Consequently, ACTOPLUS MET should not be used in patients with active bladder cancer and the benefits of glycemic control versus unknown risks for cancer recurrence with ACTOPLUS MET should be considered in patients with a prior history of bladder cancer.
5.7 Fractures
In PROactive (the Prospective Pioglitazone Clinical Trial in Macrovascular Events), 5,238 patients with type 2 diabetes mellitus and a history of macrovascular disease were randomized to pioglitazone (N=2,605), force-titrated up to 45 mg daily or placebo (N=2,633) in addition to standard of care. During a mean follow-up of 34.5 months, the incidence of bone fracture in females was 5.1% (44/870) for pioglitazone versus 2.5% (23/905) for placebo. This difference was noted after the first year of treatment and persisted during the course of the study. The majority of fractures observed in female patients were nonvertebral fractures including lower limb and distal upper limb. No increase in the incidence of fracture was observed in men treated with pioglitazone (1.7%) versus placebo (2.1%). The risk of fracture should be considered in the care of patients, especially female patients, treated with ACTOPLUS MET and attention should be given to assessing and maintaining bone health according to current standards of care.
5.8 Macular Edema
Macular edema has been reported in postmarketing experience in diabetic patients who were taking pioglitazone or another thiazolidinedione. Some patients presented with blurred vision or decreased visual acuity, but others were diagnosed on routine ophthalmologic examination.
Most patients had peripheral edema at the time macular edema was diagnosed. Some patients had improvement in their macular edema after discontinuation of the thiazolidinedione.
Patients with diabetes should have regular eye exams by an ophthalmologist according to current standards of care. Patients with diabetes who report any visual symptoms should be promptly referred to an ophthalmologist, regardless of the patient's underlying medications or other physical findings [see Adverse Reactions (6.1)].
5.9 Vitamin B12 Levels
In metformin clinical trials of 29-week duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels was observed in approximately 7% of patients. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex, may be associated with anemia but appears to be rapidly reversible with discontinuation of metformin or vitamin B12 supplementation. Certain individuals (those with inadequate vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal vitamin B12 levels. Measure hematologic parameters on an annual basis and vitamin B12 at 2 to 3 year intervals in patients on ACTOPLUS MET and manage any abnormalities [see Adverse Reactions (6.1)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed elsewhere in the labeling:
- Congestive heart failure [see Boxed Warning, Warnings and Precautions (5.1)]
- Lactic acidosis [see Boxed Warning, Warnings and Precautions (5.2)]
- Edema [see Warnings and Precautions (5.3)]
- Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues [see Warnings and Precautions (5.4)]
- Hepatic Effects [see Warnings and Precautions (5.5)]
- Urinary Bladder Tumors [see Warnings and Precautions (5.6)]
- Fractures [see Warnings and Precautions (5.7)]
- Macular Edema [see Warnings and Precautions (5.8]
- Vitamin B12 Levels [see Warnings and Precautions (5.9]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Pioglitazone
Over 8,500 patients with type 2 diabetes mellitus have been treated with pioglitazone in randomized, double-blind, controlled clinical trials, including 2,605 patients with type 2 diabetes mellitus and macrovascular disease treated with pioglitazone from the PROactive clinical trial. In these trials, over 6,000 patients have been treated with pioglitazone for six months or longer, over 4,500 patients have been treated with pioglitazone for one year or longer, and over 3,000 patients have been treated with pioglitazone for at least two years.
In six pooled 16 to 26 week placebo-controlled monotherapy and 16 to 24 week add-on combination therapy trials, the incidence of withdrawals due to adverse events was 4.5% for patients treated with pioglitazone and 5.8% for comparator-treated patients. The most common adverse events leading to withdrawal were related to inadequate glycemic control, although the incidence of these events was lower (1.5%) with pioglitazone than with placebo (3.0%).
In the PROactive trial, the incidence of withdrawals due to adverse events was 9.0% for patients treated with pioglitazone and 7.7% for placebo-treated patients. Congestive heart failure was the most common serious adverse event leading to withdrawal occurring in 1.3% of patients treated with pioglitazone and 0.6% of patients treated with placebo.
Common Adverse Events: 16 to 26 Week Monotherapy Trials
A summary of the incidence and type of common adverse events reported in three pooled 16 to 26 week placebo-controlled monotherapy trials of pioglitazone is provided in Table 2. Terms that are reported represent those that occurred at an incidence of >5% and more commonly in patients treated with pioglitazone than in patients who received placebo. None of these adverse events were related to the pioglitazone dose.
Table 2: Three Pooled 16 to 26 Week Placebo-Controlled Clinical Trials of Pioglitazone Monotherapy: Adverse Events Reported at an Incidence >5% and More Commonly in Patients Treated with Pioglitazone than in Patients Treated with Placebo % of Patients
Placebo
N=259Pioglitazone
N=606Upper Respiratory Tract Infection
8.5
13.2
Headache
6.9
9.1
Sinusitis
4.6
6.3
Myalgia
2.7
5.4
Pharyngitis
0.8
5.1
Common Adverse Events: 16 to 24 Week Add-on Combination Therapy Trials
A summary of the overall incidence and types of common adverse events reported in trials of pioglitazone add-on to metformin is provided in Table 3. Terms that are reported represent those that occurred at an incidence of >5% and more commonly with the highest tested dose of pioglitazone.
Table 3: 16 to 24 Week Clinical Trials of Pioglitazone Add-on to Metformin Note: The preferred terms of edema peripheral, generalized edema, pitting edema, and fluid retention were combined to form the aggregate term of “edema.” 16 Week Placebo-Controlled Trial
Adverse Events Reported in >5% of Patients and More Commonly in Patients Treated with Pioglitazone + Metformin
than in Patients Treated with Placebo + Metformin% of Patients
Placebo
+ Metformin
N=160Pioglitazone 30 mg
+ Metformin
N=168Edema
2.5
6.0
Headache
1.9
6.0
24 Week Non-Controlled Double-Blind Trial Adverse Events Reported in >5% of Patients and More Commonly in Patients Treated with Pioglitazone 45 mg + Metformin than in Patients Treated with Pioglitazone 30 mg + Metformin
% of Patients
Pioglitazone 30 mg
+ Metformin
N=411Pioglitazone 45 mg
+ Metformin
N=416Upper Respiratory Tract Infection
12.4
13.5
Edema
5.8
13.9
Headache
5.4
5.8
Weight Increased
2.9
6.7
Common Adverse Events: 24 Week ACTOPLUS MET Clinical Trial
Table 4 summarizes the incidence and types of adverse reactions reported in a controlled, 24 week double-blind clinical trial of ACTOPLUS MET dosed twice daily in patients with inadequate glycemic control on diet and exercise (N=600).
Table 4: Adverse Events (≥5% for ACTOPLUS MET) Reported by Patients with Inadequate Glycemic Control on Diet and Exercise in a 24 Week Double-Blind Clinical Trial of ACTOPLUS MET Administered Twice Daily % of Patients
ACTOPLUS MET
15/850 mg
Twice Daily
N=201Pioglitazone
15 mg
Twice Daily
N=190Metformin
850 mg
Twice Daily
N=209Diarrhea
9.0
2.6
15.3
Headache
5.5
2.6
4.8
In this 24 week trial, abdominal pain was reported in 2.0% of patients in the ACTOPLUS MET group, 1.6% in the pioglitazone monotherapy group and 3.3% in the metformin monotherapy group.
Common Adverse Events: PROactive Trial
A summary of the overall incidence and types of common adverse events reported in the PROactive trial is provided in Table 5. Terms that are reported represent those that occurred at an incidence of >5% and more commonly in patients treated with pioglitazone than in patients who received placebo.
Table 5: PROactive Trial: Incidence and Types of Adverse Events Reported in >5% of Patients Treated with Pioglitazone and More Commonly than Placebo Mean duration of patient follow-up was 34.5 months. % of Patients
Placebo
N=2,633Pioglitazone
N=2,605Hypoglycemia
18.8
27.3
Edema
15.3
26.7
Cardiac Failure
6.1
8.1
Pain in Extremity
5.7
6.4
Back Pain
5.1
5.5
Chest Pain
5.0
5.1
Congestive Heart Failure
A summary of the incidence of adverse events related to congestive heart failure is provided in Table 6 for the 16 to 24 week add-on to metformin trials. None of the events were fatal.
Table 6: Treatment-Emergent Adverse Events of Congestive Heart Failure (CHF) Patients Treated with Pioglitazone or Placebo Added on to Metformin Number (%) of Patients
Placebo-Controlled Trial
(16 weeks)Non-Controlled
Double-Blind Trial
(24 weeks)Placebo
+ Metformin
N=160Pioglitazone
30 mg
+ Metformin
N=168Pioglitazone
30 mg
+ Metformin
N=411Pioglitazone
45 mg
+ Metformin
N=416At least one congestive heart failure event
0
1 (0.6%)
0
1 (0.2%)
Hospitalized
0
1 (0.6%)
0
1 (0.2%)
Table 7: Treatment-Emergent Adverse Events of Congestive Heart Failure (CHF) Patients Treated with Pioglitazone or Placebo Added on to a Sulfonylurea
Number (%) of Patients
Placebo-Controlled Trial
(16 weeks)Non-Controlled Double-Blind Trial
(24 weeks)Placebo
+ Sulfonylurea
N=187Pioglitazone 15 mg
+ Sulfonylurea
N=184Pioglitazone 30 mg
+ Sulfonylurea
N=189Pioglitazone 30 mg
+ Sulfonylurea
N=351Pioglitazone 45 mg
+ Sulfonylurea
N=351At least one congestive heart failure event
2 (1.1%)
0
0
1 (0.3%)
6 (1.7%)
Hospitalized
2 (1.1%)
0
0
0
2 (0.6%)
Patients Treated with Pioglitazone or Placebo Added on to Insulin
Number (%) of Patients
Placebo-Controlled Trial
(16 weeks)Non-Controlled Double-Blind Trial (24 weeks)
Placebo
+ Insulin
N=187Pioglitazone 15 mg
+ Insulin
N=191Pioglitazone 30 mg
+ Insulin
N=188Pioglitazone 30 mg
+ Insulin
N=345Pioglitazone 45 mg
+ Insulin
N=345At least one congestive heart failure event
0
2 (1.0%)
2 (1.1%)
3 (0.9%)
5 (1.4%)
Hospitalized
0
2 (1.0%)
1 (0.5%)
1 (0.3%)
3 (0.9%)
Patients Treated with Pioglitazone or Placebo Added on to Metformin
Number (%) of Patients
Placebo-Controlled Trial
(16 weeks)Non-Controlled Double-Blind Trial
(24 weeks)Placebo
+ Metformin
N=160Pioglitazone
30 mg
+ Metformin
N=168Pioglitazone 30 mg
+ Metformin
N=411Pioglitazone 45 mg
+ Metformin
N=416At least one congestive heart failure event
0
1 (0.6%)
0
1 (0.2%)
Hospitalized
0
1 (0.6%)
0
1 (0.2%)
Table 8: Treatment-Emergent Adverse Events of Congestive Heart Failure (CHF) in Patients with NYHA Class II or III Congestive Heart Failure Treated with Pioglitazone or Glyburide Number (%) of Subjects
Pioglitazone
N=262Glyburide
N=256Death due to cardiovascular causes (adjudicated)
5 (1.9%)
6 (2.3%)
Overnight hospitalization for worsening CHF (adjudicated)
26 (9.9%)
12 (4.7%)
Emergency room visit for CHF (adjudicated)
4 (1.5%)
3 (1.2%)
Patients experiencing CHF progression during study
35 (13.4%)
21 (8.2%)
Congestive heart failure events leading to hospitalization that occurred during the PROactive trial are summarized in Table 9.
Table 9: Treatment-Emergent Adverse Events of Congestive Heart Failure (CHF) in PROactive Trial Number (%) of Patients
Placebo
N=2,633Pioglitazone
N=2,605At least one hospitalized congestive heart failure event
108 (4.1%)
149 (5.7%)
Fatal
22 (0.8%)
25 (1.0%)
Hospitalized, nonfatal
86 (3.3%)
124 (4.7%)
Cardiovascular Safety
In the PROactive trial, 5,238 patients with type 2 diabetes mellitus and a history of macrovascular disease were randomized to pioglitazone (N=2,605), force-titrated up to 45 mg daily or placebo (N=2,633) in addition to standard of care. Almost all patients (95%) were receiving cardiovascular medications (beta blockers, ACE inhibitors, angiotensin II receptor blockers, calcium channel blockers, nitrates, diuretics, aspirin, statins, and fibrates). At baseline, patients had a mean age of 62 years, mean duration of diabetes of 9.5 years, and mean HbA1c of 8.1%. Mean duration of follow-up was 34.5 months.
The primary objective of this trial was to examine the effect of pioglitazone on mortality and macrovascular morbidity in patients with type 2 diabetes mellitus who were at high risk for macrovascular events. The primary efficacy variable was the time to the first occurrence of any event in a cardiovascular composite endpoint that included all-cause mortality, nonfatal myocardial infarction (MI) including silent MI, stroke, acute coronary syndrome, cardiac intervention including coronary artery bypass grafting or percutaneous intervention, major leg amputation above the ankle, and bypass surgery or revascularization in the leg. A total of 514 (19.7%) patients treated with pioglitazone and 572 (21.7%) placebo-treated patients experienced at least one event from the primary composite endpoint (HR = 0.90; 95% CI: 0.80, 1.02; p=0.10).
Although there was no statistically significant difference between pioglitazone and placebo for the three year incidence of a first event within this composite, there was no increase in mortality or in total macrovascular events with pioglitazone. The number of first occurrences and total individual events contributing to the primary composite endpoint is shown in Table 10.
Table 10: PROactive Trial: Number of First and Total Events for Each Component Within the Cardiovascular Composite Endpoint CABG = coronary artery bypass grafting; PCI = percutaneous intervention. Cardiovascular Events
Placebo
N=2,633Pioglitazone
N=2,605First
Events
n (%)Total events
nFirst
Events
n (%)Total events
nAny event
572 (21.7)
900
514 (19.7)
803
All-cause mortality
122 (4.6)
186
110 (4.2)
177
Nonfatal myocardial infarction (MI)
118 (4.5)
157
105 (4.0)
131
Stroke
96 (3.6)
119
76 (2.9)
92
Acute coronary syndrome
63 (2.4)
78
42 (1.6)
65
Cardiac intervention (CABG/PCI)
101 (3.8)
240
101 (3.9)
195
Major leg amputation
15 (0.6)
28
9 (0.3)
28
Leg revascularization
57 (2.2)
92
71 (2.7)
115
Weight Gain
Dose-related weight gain occurs when pioglitazone is used alone or in combination with other antidiabetic medications. The mechanism of weight gain is unclear but probably involves a combination of fluid retention and fat accumulation.
Tables 11, 12, and 13 summarize the changes in body weight with pioglitazone and placebo in the 16 to 26 week randomized, double-blind monotherapy and 16 to 24 week combination add-on therapy trials, the PROactive trial, and the 24 week ACTOPLUS MET trial.
Table 11: Weight Changes (kg) from Baseline During Randomized, Double-Blind Clinical Trials Control Group
(Placebo)Pioglitazone
15 mgPioglitazone
30 mgPioglitazone
45 mgMedian
(25th, 75th percentile)Median
(25th, 75th percentile)Median
(25th, 75th percentile)Median
(25th, 75th percentile)Monotherapy
(16 to 26 weeks)-1.4 (-2.7, 0.0)
N=2560.9 (-0.5, 3.4)
N=791.0 (-0.9, 3.4)
N=1882.6 (0.2, 5.4)
N=79
Combination
Therapy
(16 to 24 weeks)Sulfonylurea
-0.5 (-1.8, 0.7)
N=1872.0 (0.2, 3.2)
N=1833.1 (1.1, 5.4)
N=5284.1 (1.8, 7.3)
N=333Metformin
-1.4 (-3.2, 0.3)
N=160N/A
0.9 (-1.3, 3.2)
N=5671.8 (-0.9, 5.0)
N=407Insulin
0.2 (-1.4, 1.4)
N=1822.3 (0.5, 4.3)
N=1903.3 (0.9, 6.3)
N=5224.1 (1.4, 6.8)
N=338Table 12: Median Change in Body Weight in Patients Treated with Pioglitazone vs Patients Treated with Placebo During the Double-Blind Treatment Period in the PROactive Trial Note: Median exposure for both pioglitazone and placebo was 2.7 years. Placebo
Pioglitazone
Median
(25th, 75th
percentile)Median
(25th, 75th
percentile)Change from baseline to final visit (kg)
-0.5 (-3.3, 2.0)
N=2,581+3.6 (0.0, 7.5)
N=2,560Table 13: Weight Changes (kg) from Baseline During Double-Blind Clinical Trial with ACTOPLUS MET in Patients with Inadequate Glycemic Control on Diet and Exercise Note: Trial duration of 24 weeks. ACTOPLUS MET
15/850 mg
Twice DailyPioglitazone 15 mg
Twice DailyMetformin
850 mg
Twice DailyMedian
(25th, 75th
percentile)Median
(25th, 75th
percentile)Median
(25th, 75th
percentile)Change from baseline to final visit (kg)
1.00 (-1.0, 3.0)
N=1981.35 (-0.7, 4.1)
N=178-1.00 (-2.6, 0.4)
N=203Edema
Edema induced from taking pioglitazone is reversible when pioglitazone is discontinued. The edema usually does not require hospitalization unless there is co-existing congestive heart failure.
In the 24 week ACTOPLUS MET trial, edema was reported in 3.0% of patients in the ACTOPLUS MET group, 4.2% in the pioglitazone monotherapy group, and 1.4% in the metformin monotherapy group.
A summary of the frequency and types of edema adverse events occurring in clinical investigations of pioglitazone is provided in Table 14.
Table 14: Adverse Events of Edema in Patients Treated with Pioglitazone Note: The preferred terms of edema peripheral, generalized edema, pitting edema, and fluid retention were combined to form the aggregate term of “edema.” Number (%) of Patients
Placebo
Pioglitazone
15 mgPioglitazone
30 mgPioglitazone
45 mgMonotherapy
(16 to 26 weeks)3 (1.2%)
N=2592 (2.5%)
N= 8113 (4.7%)
N= 27511 (6.5%)
N=169Combined Therapy
(16 to 24 weeks)Sulfonylurea
4 (2.1%)
N=1873 (1.6%)
N=18461 (11.3%)
N=54081 (23.1%)
N=351Metformin
4 (2.5%)
N=160N/A
34 (5.9%)
N=57958 (13.9%)
N=416Insulin
13 (7.0%)
N=18724 (12.6%)
N=191109 (20.5%)
N=53390 (26.1%)
N=345Table 15: Adverse Events of Edema in Patients in the PROactive Trial Note: The preferred terms of edema peripheral, generalized edema, pitting edema, and fluid retention were combined to form the aggregate term of “edema.” Number (%) of Patients
Placebo
N=2,633Pioglitazone
N=2,605419 (15.9%)
712 (27.3%)
Hepatic Effects
There has been no evidence of pioglitazone-induced hepatotoxicity in the pioglitazone controlled clinical trial database to date. One randomized, double-blind, three year trial comparing pioglitazone to glyburide as add-on to metformin and insulin therapy was specifically designed to evaluate the incidence of serum ALT elevation to greater than three times the upper limit of the reference range, measured every eight weeks for the first 48 weeks of the trial then every 12 weeks thereafter. A total of 3/1,051 (0.3%) patients treated with pioglitazone and 9/1,046 (0.9%) patients treated with glyburide developed ALT values greater than three times the upper limit of the reference range. None of the patients treated with pioglitazone in the pioglitazone controlled clinical trial database to date have had a serum ALT greater than three times the upper limit of the reference range and a corresponding total bilirubin greater than two times the upper limit of the reference range, a combination predictive of the potential for severe drug-induced liver injury.
Hypoglycemia
In the pioglitazone clinical trials, adverse events of hypoglycemia were reported based on clinical judgment of the investigators and did not require confirmation with fingerstick glucose testing.
In the 16 week add-on to sulfonylurea trial, the incidence of reported hypoglycemia was 3.7% with pioglitazone 30 mg and 0.5% with placebo. In the 16 week add-on to insulin trial, the incidence of reported hypoglycemia was 7.9% with pioglitazone 15 mg, 15.4% with pioglitazone 30 mg, and 4.8% with placebo.
The incidence of reported hypoglycemia was higher with pioglitazone 45 mg compared to pioglitazone 30 mg in both the 24 week add-on to sulfonylurea trial (15.7% vs 13.4%) and in the 24-week add-on to insulin trial (47.8% vs 43.5%).
Three patients in these four trials were hospitalized due to hypoglycemia. All three patients were receiving pioglitazone 30 mg (0.9%) in the 24 week add-on to insulin trial. An additional 14 patients reported severe hypoglycemia (defined as causing considerable interference with patient's usual activities) that did not require hospitalization. These patients were receiving pioglitazone 45 mg in combination with sulfonylurea (n=2) or pioglitazone 30 mg or 45 mg in combination with insulin (n=12).
Urinary Bladder Tumors
Tumors were observed in the urinary bladder of male rats in the two year carcinogenicity study [see Nonclinical Toxicology (13.1)]. During the three-year PROactive clinical trial, 14 patients out of 2,605 (0.54%) randomized to pioglitazone and 5 out of 2,633 (0.19%) randomized to placebo were diagnosed with bladder cancer. After excluding patients in whom exposure to study drug was less than one year at the time of diagnosis of bladder cancer, there were 6 (0.23%) cases on pioglitazone and 2 (0.08%) cases on placebo. After completion of the trial, a large subset of patients was observed for up to 10 additional years, with little additional exposure to pioglitazone. During the 13 years of both PROactive and observational follow-up, the occurrence of bladder cancer did not differ between patients randomized to pioglitazone or placebo (HR = 1.00; [95% CI: 0.59 1.72]) [see Warnings and Precautions (5.6)].
Metformin HCl
In a double-blind clinical study of metformin in patients with type 2 diabetes mellitus, a total of 141 patients received metformin therapy (up to 2,550 mg per day) and 145 patients received placebo. Adverse reactions reported in greater than 5% of the metformin patients, and that were more common in metformin than placebo-treated patients, are listed in Table 16. In this trial, diarrhea led to discontinuation of study medication in 6% of patients treated with metformin.
Table 16: Most Common Adverse Reactions (>5.0%) in a Placebo-Controlled Clinical Study of Metformin Monotherapy* - *
- Reactions that were more common in metformin than placebo-treated patients.
Adverse Reaction
Metformin Monotherapy
(n=141)Placebo
(n=145)% of Patients
Diarrhea
53.2
11.7
Nausea/Vomiting
25.5
8.3
Flatulence
12.1
5.5
Asthenia
9.2
5.5
Indigestion
7.1
4.1
Abdominal Discomfort
6.4
4.8
Headache
5.7
4.8
Laboratory Abnormalities
Pioglitazone
Hematologic Effects
Pioglitazone may cause decreases in hemoglobin and hematocrit. In placebo-controlled monotherapy trials, mean hemoglobin values declined by 2% to 4% in patients treated with pioglitazone compared with a mean change in hemoglobin of -1% to +1% in placebo-treated patients. These changes primarily occurred within the first four to 12 weeks of therapy and remained relatively constant thereafter. These changes may be related to increased plasma volume associated with pioglitazone therapy and are not likely to be associated with any clinically significant hematologic effects.
Creatine Phosphokinase
During protocol-specified measurement of serum creatine phosphokinase (CPK) in pioglitazone clinical trials, an isolated elevation in CPK to greater than 10 times the upper limit of the reference range was noted in nine (0.2%) patients treated with pioglitazone (values of 2,150 to 11,400 IU/L) and in no comparator-treated patients. Six of these nine patients continued to receive pioglitazone, two patients were noted to have the CPK elevation on the last day of dosing, and one patient discontinued pioglitazone due to the elevation. These elevations resolved without any apparent clinical sequelae. The relationship of these events to pioglitazone therapy is unknown.
Metformin
Vitamin B12 Concentrations
In metformin clinical trials of 29-week duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels was observed in approximately 7% of patients.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of pioglitazone and/or metformin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Pioglitazone
Cardiac Disorders: Rapid increases in weight, edema, congestive heart failure with and without previously known heart disease or concomitant insulin administration
Eye Disorders: New onset or worsening diabetic macular edema with decreased visual acuity
Hepatobiliary Disorders: Fatal and nonfatal hepatic failure
Metformin
Hepatobiliary Disorders: Cholestatic, hepatocellular, and mixed hepatocellular liver injury.
-
7 DRUG INTERACTIONS
7.1 Strong CYP2C8 Inhibitors
An inhibitor of CYP2C8 (e.g., gemfibrozil) significantly increases the exposure (area under the serum concentration-time curve or AUC) and half-life (t½) of pioglitazone. Therefore, the maximum recommended dosage of ACTOPLUS MET is 15 mg of pioglitazone and 850 mg of metformin HCl once daily if used in combination with gemfibrozil or other strong CYP2C8 inhibitors [see Dosage and Administration (2.3), Clinical Pharmacology (12.3)].
7.2 CYP2C8 Inducers
An inducer of CYP2C8 (e.g., rifampin) may significantly decrease the exposure (AUC) of pioglitazone. Therefore, if an inducer of CYP2C8 is started or stopped during treatment with ACTOPLUS MET, changes in diabetes treatment may be needed based on clinical response without exceeding the maximum recommended daily dosage of ACTOPLUS MET (45 mg of pioglitazone and 2,550 mg of metformin HCl) [see Clinical Pharmacology (12.3)].
7.3 Carbonic Anhydrase Inhibitors
Topiramate or other carbonic anhydrse inhibitors (e.g., zonisamide, acetazolamide or dichlorphenamide) frequently causes a decrease in serum bicarbonate and induce non-anion gap, hyperchloremic metabolic acidosis. Concomitant use of these drugs with ACTOPLUS MET may increase the risk for lactic acidosis. Consider more frequent monitoring of these patients.
7.4 Drugs that Reduce Metformin Clearance
Concomitant use of drugs that interfere with common renal tubular transport systems involved in the renal elimination of metformin (e.g., organic cationic transporter-2 [OCT2]/multidrug and toxin extrusion [MATE] inhibitors such as ranolazine, vandetanib, dolutegravir, and cimetidine) could increase systemic exposure to metformin and may increase the risk for lactic acidosis [see Clinical Pharmacology (12.3)]. Consider the benefits and risks of concomitant use.
7.5 Alcohol
Alcohol is known to potentiate the effect of metformin on lactate metabolism. Warn patients against excessive alcohol intake while receiving ACTOPLUS MET.
7.6 Insulin Secretagogues or Insulin
Coadministration of ACTOPLUS MET with an insulin secretagogue (e.g., sulfonylurea) or insulin may increase the risk of hypoglycemia. If hypoglycemia occurs in a patient coadministered ACTOPLUS MET and an insulin secretagogue (e.g., sulfonylurea), the dose of the insulin secretagogue should be reduced.
7.7 Drugs Affecting Glycemic Control
Certain drugs tend to produce hyperglycemia and may lead to loss of glycemic control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel blockers, and isoniazid. When such drugs are administered to a patient receiving ACTOPLUS MET, the patient should be closely observed for loss of blood glucose control. When such drugs are withdrawn from a patient receiving ACTOPLUS MET, the patient should be observed closely for hypoglycemia.
7.8 Topiramate
A decrease in the exposure of pioglitazone and its active metabolites were noted with concomitant administration of pioglitazone and topiramate [see Clinical Pharmacology (12.3)]. The clinical relevance of this decrease is unknown; however, when ACTOPLUS MET and topiramate are used concomitantly, monitor patients for adequate glycemic control.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited data with ACTOPLUS MET or pioglitazone in pregnant women are not sufficient to determine a drug-associated risk for major birth defects or miscarriage. Published studies with metformin use during pregnancy have not reported a clear association with metformin and major birth defect or miscarriage risk (see Data). There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy [see Clinical Considerations].
In animal reproduction studies, no adverse developmental effects were observed when pioglitazone was administered to pregnant rats and rabbits during organogenesis at exposures up to 5 and 35 times the 45 mg clinical dose, respectively, based on body surface area. No adverse developmental effects were observed when metformin was administered to pregnant Sprague Dawley rats and rabbits during the period of organogenesis at doses up to 2 to 6 times, respectively, a 2,000 mg clinical dose, based on body surface area (see Data).
The estimated background risk of major birth defects is 6 to 10% in women with pre-gestational diabetes with a HbA1c >7 and has been reported to be as high as 20 to 25% in women with a HbA1c >10. The estimated background risk of miscarriage for the indicated population is unknown. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Poorly controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis, pre-eclampsia, spontaneous abortions, preterm delivery, still birth and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, still birth, and macrosomia related morbidity.
Data
Human Data
Published data from postmarketing studies have not reported a clear association with metformin and major birth defects, miscarriage, or adverse maternal or fetal outcomes when metformin was used during pregnancy. However, these studies cannot definitely establish the absence of any metformin-associated risk because of methodological limitations, including small sample size and inconsistent comparator groups.
Animal Data
Pioglitazone and Metformin HCl
Animal reproduction studies were not conducted with the combined products in ACTOPLUS MET. The following data are based on studies conducted with the individual components of ACTOPLUS MET.
Pioglitazone
Pioglitazone administered to pregnant rats during organogenesis did not cause adverse developmental effects at a dose of 20 mg/kg (~5 times the 45 mg clinical dose), but delayed parturition and reduced embryo-fetal viability at 40 and 80 mg/kg, or ≥9 times the 45 mg clinical dose, by body surface area. In pregnant rabbits administered pioglitazone during organogenesis, no adverse developmental effects were observed at 80 mg/kg (~35 times the 45 mg clinical dose), but reduced embryo-fetal viability at 160 mg/kg, or ~69 times the 45 mg clinical dose, by body surface area. When pregnant rats received pioglitazone during late gestation and lactation, delayed postnatal development, attributed to decreased body weight, occurred in offspring at maternal doses of 10 mg/kg and above or ≥2 times the 45 mg clinical dose, by body surface area.
Metformin HCl
Metformin HCl did not cause adverse developmental effects when administered to pregnant Sprague Dawley rats and rabbits up to 600 mg/kg/day during the period of organogenesis. This represents an exposure of about 2 to 6 times a 2,000 mg clinical dose based on body surface area (mg/m2) for rats and rabbits, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of ACTOPLUS MET or pioglitazone in human milk, the effects on the breastfed infant, or the effects on milk production. Pioglitazone is present in rat milk; however, due to species-specific differences in lactation physiology, animal data may not reliably predict drug levels in human milk. Limited published studies report that metformin is present in human milk (see Data). However, there is insufficient information on the effects of metformin on the breastfed infant and no available information on the effects of metformin on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ACTOPLUS MET and any potential adverse effects on the breastfed infant from ACTOPLUS MET or from the underlying maternal condition.
Data
Published clinical lactation studies report that metformin is present in human milk which resulted in infant doses approximately 0.11% to 1% of the maternal weight-adjusted dosage and a milk/plasma ratio ranging between 0.13 and 1. However, the studies were not designed to definitely establish the risk of use of metformin during lactation because of small sample size and limited adverse event data collected in infants.
8.3 Females and Males of Reproductive Potential
Discuss the potential for unintended pregnancy with premenopausal women as therapy with ACTOPLUS MET, may result in ovulation in some anovulatory women.
8.4 Pediatric Use
Safety and effectiveness of ACTOPLUS MET in pediatric patients have not been established.
ACTOPLUS MET is not recommended for use in pediatric patients based on adverse effects observed in adults, including fluid retention and congestive heart failure, fractures, and urinary bladder tumors [see Warnings and Precautions (5.1, 5.3, 5.6, 5.7)].
8.5 Geriatric Use
Pioglitazone
A total of 92 patients (15.2%) treated with pioglitazone in the three pooled 16 to 26 week double-blind, placebo-controlled, monotherapy trials were ≥65 years old and two patients (0.3%) were ≥75 years old. In the two pooled 16 to 24 week add-on to sulfonylurea trials, 201 patients (18.7%) treated with pioglitazone were ≥65 years old and 19 (1.8%) were ≥75 years old. In the two pooled 16 to 24 week add-on to metformin trials, 155 patients (15.5%) treated with pioglitazone were ≥65 years old and 19 (1.9%) were ≥75 years old. In the two pooled 16 to 24 week add-on to insulin trials, 272 patients (25.4%) treated with pioglitazone were ≥65 years old and 22 (2.1%) were ≥75 years old.
In PROactive Trial, 1,068 patients (41.0%) treated with pioglitazone were ≥65 years old and 42 (1.6%) were ≥75 years old.
In pharmacokinetic studies with pioglitazone, no significant differences were observed in pharmacokinetic parameters between elderly and younger patients [see Clinical Pharmacology (12.3)].
Although clinical experiences have not identified differences in effectiveness and safety between the elderly (≥65 years) and younger patients, these conclusions are limited by small sample sizes for patients ≥75 years old.
Metformin HCl
Controlled clinical studies of metformin did not include sufficient numbers of elderly patients to determine whether they respond differently from younger patients, although other reported clinical experience has not identified differences in responses between the elderly and young patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy and the higher risk of lactic acidosis. Assess renal function more frequently in elderly patients [see Warnings and Precautions (5.2), Dosage and Administration (2.2)].
8.6 Renal Impairment
Metformin is substantially excreted by the kidney, and the risk of metformin accumulation and lactic acidosis increases with the degree of renal impairment. ACTOPLUS MET is contraindicated in severe renal impairment, which includes patients with an eGFR below 30 mL/min [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.2), Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Use of metformin in patients with hepatic impairment has been associated with some cases of lactic acidosis. ACTOPLUS MET is not recommended in patients with hepatic impairment [see Warnings and Precautions (5.2)].
-
10 OVERDOSAGE
Pioglitazone
During controlled clinical trials, one case of overdose with pioglitazone was reported. A male patient took 120 mg per day for four days, then 180 mg per day for seven days. The patient denied any clinical symptoms during this period.
Metformin HCl
Overdose of metformin HCl has occurred, including ingestion of amounts greater than 50 grams. Hypoglycemia was reported in approximately 10% of cases, but no causal association with metformin HCl has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases [see Warnings and Precautions (5.2)]. Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated metformin from patients in whom metformin overdosage is suspected.
In the event of overdosage, contact the Poison Help Line (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations. Appropriate supportive treatment should be initiated according to the patient’s clinical signs and symptoms.
-
11 DESCRIPTION
ACTOPLUS MET tablets are a thiazolidinediones and biguanide combination product that contains two oral antidiabetic medications: pioglitazone HCl and metformin HCl.
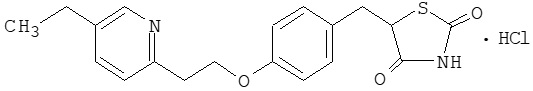
Pioglitazone [(±)-5-[[4-[2-(5-ethyl-2-pyridinyl) ethoxy]phenyl]methyl]-2,4-] thiazolidinedione monohydrochloride contains one asymmetric carbon, and the compound is synthesized and used as the racemic mixture. The two enantiomers of pioglitazone interconvert in vivo. No differences were found in the pharmacologic activity between the two enantiomers. The structural formula is as shown:
Pioglitazone HCl is an odorless white crystalline powder that has a molecular formula of C19H20N2O3S•HCl and a molecular weight of 392.90 daltons. It is soluble in N,N-dimethylformamide, slightly soluble in anhydrous ethanol, very slightly soluble in acetone and acetonitrile, practically insoluble in water, and insoluble in ether.
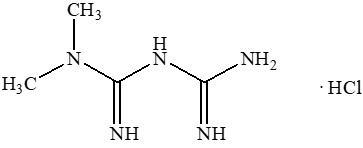
Metformin HCl (N,N-dimethylimidodicarbonimidic diamide HCl) is a white crystalline powder with a molecular formula of C4H11N5•HCl and a molecular weight of 165.62. Metformin HCl is freely soluble in water and is practically insoluble in acetone, ether, and chloroform. The pKa of metformin is 12.4. The pH of a 1% aqueous solution of metformin HCl is 6.68. The structural formula is as shown:
ACTOPLUS MET is available as a tablet for oral administration containing 15 mg pioglitazone (as the base) with 850 mg metformin HCl (15 mg/850 mg) formulated with the following excipients: povidone USP, microcrystalline cellulose NF, croscarmellose sodium NF, magnesium stearate NF, hypromellose 2910 USP, polyethylene glycol 8000 NF, titanium dioxide USP, and talc USP.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
ACTOPLUS MET combines two antihyperglycemic agents: pioglitazone and metformin.
Pioglitazone
Pioglitazone is a thiazolidinedione that depends on the presence of insulin for its mechanism of action. Pioglitazone decreases insulin resistance in the periphery and in the liver resulting in increased insulin-dependent glucose disposal and decreased hepatic glucose output. Pioglitazone is not an insulin secretagogue. Pioglitazone is an agonist for peroxisome proliferator-activated receptor-gamma (PPARγ). PPAR receptors are found in tissues important for insulin action such as adipose tissue, skeletal muscle, and liver. Activation of PPARγ nuclear receptors modulates the transcription of a number of insulin responsive genes involved in the control of glucose and lipid metabolism.
In animal models of diabetes, pioglitazone reduces the hyperglycemia, hyperinsulinemia, and hypertriglyceridemia characteristic of insulin-resistant states such as type 2 diabetes mellitus. The metabolic changes produced by pioglitazone result in increased responsiveness of insulin-dependent tissues and are observed in numerous animal models of insulin resistance.
Because pioglitazone enhances the effects of circulating insulin (by decreasing insulin resistance), it does not lower blood glucose in animal models that lack endogenous insulin.
Metformin HCl
Metformin HCl improves glucose tolerance in patients with type 2 diabetes mellitus, lowering both basal and postprandial plasma glucose. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. Metformin does not produce hypoglycemia in either patients with type 2 diabetes mellitus or healthy subjects [except in specific circumstances, see Warnings and Precautions (5.4)] and does not cause hyperinsulinemia. With metformin therapy, insulin secretion remains unchanged while fasting insulin levels and day-long plasma insulin response may actually decrease.
12.2 Pharmacodynamics
Pioglitazone
Clinical studies demonstrate that pioglitazone improves insulin sensitivity in insulin-resistant patients. Pioglitazone enhances cellular responsiveness to insulin, increases insulin-dependent glucose disposal and improves hepatic sensitivity to insulin. In patients with type 2 diabetes mellitus, the decreased insulin resistance produced by pioglitazone results in lower plasma glucose concentrations, lower plasma insulin concentrations, and lower HbA1c values. In controlled clinical trials, pioglitazone had an additive effect on glycemic control when used in combination with a sulfonylurea, metformin, or insulin [see Clinical Studies (14)].
Patients with lipid abnormalities were included in clinical trials with pioglitazone. Overall, patients treated with pioglitazone had mean decreases in serum triglycerides, mean increases in HDL cholesterol, and no consistent mean changes in LDL and total cholesterol. There is no conclusive evidence of macrovascular benefit with pioglitazone [see Adverse Reactions (6.1)].
In a 26 week, placebo-controlled, dose-ranging monotherapy study, mean serum triglycerides decreased in the 15 mg, 30 mg, and 45 mg pioglitazone dose groups compared to a mean increase in the placebo group. Mean HDL cholesterol increased to a greater extent in patients treated with pioglitazone than in the placebo-treated patients. There were no consistent differences for LDL and total cholesterol in patients treated with pioglitazone compared to placebo (see Table 17).
Table 17: Lipids in a 26 Week Placebo-Controlled Monotherapy Dose-Ranging Study Placebo
Pioglitazone
15 mg
Once
DailyPioglitazone
30 mg
Once
DailyPioglitazone
45 mg
Once
DailyTriglycerides (mg/dL)
N=79
N=79
N=84
N=77
Baseline (mean)
263
284
261
260
Percent change from baseline (adjusted mean*)
4.8%
-9.0%†
-9.6%†
-9.3%†
HDL Cholesterol (mg/dL)
N=79
N=79
N=83
N=77
Baseline (mean)
42
40
41
41
Percent change from baseline (adjusted mean*)
8.1%
14.1%†
12.2%
19.1%†
LDL Cholesterol (mg/dL)
N=65
N=63
N=74
N=62
Baseline (mean)
139
132
136
127
Percent change from baseline (adjusted mean*)
4.8%
7.2%
5.2%
6.0%
Total Cholesterol (mg/dL)
N=79
N=79
N=84
N=77
Baseline (mean)
225
220
223
214
Percent change from baseline (adjusted mean*)
4.4%
4.6%
3.3%
6.4%
In the two other monotherapy studies (16 weeks and 24 weeks) and in combination therapy studies with metformin (16 weeks and 24 weeks), the results were generally consistent with the data above.
12.3 Pharmacokinetics
Absorption
ACTOPLUS MET
In bioequivalence studies of ACTOPLUS MET 15 mg/500 mg and 15 mg/850 mg, the area under the curve (AUC) and maximum concentration (Cmax) of both the pioglitazone and the metformin component following a single dose of the combination tablet were bioequivalent to ACTOS 15 mg concomitantly administered with metformin HCl immediate release (500 mg or 850 mg, respectively) tablets under fasted conditions in healthy subjects.
Administration of ACTOPLUS MET 15 mg/850 mg with food resulted in no change in overall exposure of pioglitazone. With metformin there was no change in AUC; however, mean peak serum concentration of metformin was decreased by 28% when administered with food. A delayed time to peak serum concentration was observed for both components (1.9 hours for pioglitazone and 0.8 hours for metformin) under fed conditions. These changes are not likely to be clinically significant.
Pioglitazone
Following once-daily administration of pioglitazone, steady-state serum concentrations of both pioglitazone and its major active metabolites, M-III (keto derivative of pioglitazone) and M-IV (hydroxyl derivative of pioglitazone), are achieved within seven days. At steady state, M-III and M-IV reach serum concentrations equal to or greater than that of pioglitazone. At steady state, in both healthy volunteers and patients with type 2 diabetes mellitus, pioglitazone comprises approximately 30 to 50% of the peak total pioglitazone serum concentrations (pioglitazone plus active metabolites) and 20 to 25% of the total AUC.
Cmax, AUC, and trough serum concentrations (Cmin) for pioglitazone and M-III and M-IV, increased proportionally with administered doses of 15 mg and 30 mg per day.
Following oral administration of pioglitazone, Tmax of pioglitazone was within two hours. Food delays the Tmax to three to four hours, but does not alter the extent of absorption (AUC).
Metformin HCl
The absolute bioavailability of a 500 mg metformin tablet given under fasting conditions is approximately 50 to 60%. Studies using single oral doses of metformin tablets of 500 mg to 1500 mg, and 850 mg to 2,550 mg, indicate that there is a lack of dose proportionality with increasing doses, which is due to decreased absorption rather than an alteration in elimination. At usual clinical doses and dosing schedules of metformin, steady-state plasma concentrations of metformin are reached within 24 to 48 hours and are generally <1 mcg/mL. During controlled clinical trials, maximum metformin plasma levels did not exceed 5 mcg/mL, even at maximum doses.
Food decreases the rate and extent of metformin absorption, as shown by a 40% lower mean Cmax, a 25% lower AUC, and a 35 minute prolongation of Tmax following administration of a single 850 mg tablet of metformin with food, compared to the same tablet strength administered fasting. The clinical relevance of these decreases is unknown.
Distribution
Pioglitazone
The mean apparent volume of distribution (Vd/F) of pioglitazone following single-dose administration is 0.63 ± 0.41 (mean ± SD) L/kg of body weight. Pioglitazone is extensively protein bound (>99%) in human serum, principally to serum albumin. Pioglitazone also binds to other serum proteins, but with lower affinity. M-III and M-IV are also extensively bound (>98%) to serum albumin.
Metformin HCl
The Vd/F of metformin following single oral doses of 850 mg immediate-release metformin averaged 654 ± 358 L. Metformin is negligibly bound to plasma proteins. Metformin partitions into erythrocytes, most likely as a function of time.
Elimination
Metabolism
Pioglitazone
Pioglitazone is extensively metabolized by hydroxylation and oxidation; the metabolites also partly convert to glucuronide or sulfate conjugates. Metabolites M-III and M-IV are the major circulating active metabolites in humans.
In vitro data demonstrate that multiple CYP isoforms are involved in the metabolism of pioglitazone which include CYP2C8 and, to a lesser degree, CYP3A4 with additional contributions from a variety of other isoforms, including the mainly extrahepatic CYP1A1. In vivo study of pioglitazone in combination with gemfibrozil, a strong CYP2C8 inhibitor, showed that pioglitazone is a CYP2C8 substrate [see Dosage and Administration (2.3), Drug Interactions (7.1)]. Urinary 6ß-hydroxycortisol/cortisol ratios measured in patients treated with pioglitazone showed that pioglitazone is not a strong CYP3A4 enzyme inducer.
Metformin HCl
Intravenous single-dose studies in healthy subjects demonstrate that metformin is excreted unchanged in the urine and does not undergo hepatic metabolism (no metabolites have been identified in humans) nor biliary excretion.
Excretion
Pioglitazone
Following oral administration, approximately 15 to 30% of the pioglitazone dose is recovered in the urine. Renal elimination of pioglitazone is negligible and the drug is excreted primarily as metabolites and their conjugates. It is presumed that most of the oral dose is excreted into the bile either unchanged or as metabolites and eliminated in the feces.
The mean serum half-life (t½) of pioglitazone and its metabolites (M-III and M-IV) range from three to seven hours and 16 to 24 hours, respectively. Pioglitazone has an apparent clearance, CL/F, calculated to be five to seven L/hr.
Metformin HCl
Renal clearance is approximately 3.5 times greater than creatinine clearance (CrCl), which indicates that tubular secretion is the major route of metformin elimination. Following oral administration, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination t½ of approximately 6.2 hours. In blood, the elimination t½ is approximately 17.6 hours, suggesting that the erythrocyte mass may be a compartment of distribution.
Specific Populations
Geriatric Patients
Pioglitazone
In healthy elderly subjects, Cmax of pioglitazone was not significantly different, but AUC values were approximately 21% higher than those achieved in younger subjects. The mean t½ of pioglitazone was also prolonged in elderly subjects (about ten hours) as compared to younger subjects (about seven hours). These changes are not considered clinically relevant.
Metformin HCl
Limited data from controlled pharmacokinetic studies of metformin in healthy elderly subjects suggest that total CL/F is decreased, the t½ is prolonged, and Cmax is increased, compared to healthy young subjects. From these data, it appears that the change in metformin pharmacokinetics with aging is primarily accounted for by a change in renal function.
Pediatric Patients
Pioglitazone
Safety and efficacy of pioglitazone in pediatric patients have not been established. ACTOPLUS MET is not recommended for use in pediatric patients [see Use in Specific Populations (8.4)].
Metformin HCl
After administration of a single oral metformin 500 mg tablet with food, geometric mean metformin Cmax and AUC differed less than 5% between pediatric type 2 diabetic patients (12 to 16 years of age) and gender- and weight-matched healthy adults (20 to 45 years of age), and all with normal renal function.
Male and Female Patients
Pioglitazone
The mean Cmax and AUC values of pioglitazone were increased 20 to 60% in females compared to males. In controlled clinical trials, HbA1c decreases from baseline were generally greater for females than for males (average mean difference in HbA1c 0.5%). Because therapy should be individualized for each patient to achieve glycemic control, no dosage adjustment is recommended based on gender alone.
Metformin HCl
Metformin pharmacokinetic parameters did not differ significantly between normal subjects and patients with type 2 diabetes mellitus when analyzed according to gender (males=19, females=16). Similarly, in controlled clinical studies in patients with type 2 diabetes mellitus, the antihyperglycemic effect of metformin was comparable in males and females.
Racial or Ethnic Groups
Pioglitazone
Pharmacokinetic data among various ethnic groups are not available.
Metformin HCl
No studies of metformin pharmacokinetic parameters according to race have been performed. In controlled clinical studies of metformin in patients with type 2 diabetes mellitus, the antihyperglycemic effect was comparable in Whites (n=249), Blacks or African Americans (n=51), and Hispanics or Latinos (n=24).
Patients with Renal Impairment
Pioglitazone
The serum elimination half-life of pioglitazone, M-III and M-IV remains unchanged in patients with moderate (CrCl 30 to 50 mL/min) and severe (CrCl <30 mL/min) renal impairment when compared to subjects with normal renal function. Therefore, no dosage adjustment in patients with renal impairment is required.
Metformin HCl
In patients with decreased renal function, the plasma and blood t1/2 of metformin is prolonged and the renal clearance is decreased [see Dosage and Administration (2.3), Contraindications (4), Warnings and Precautions (5.2)].
Patients with Hepatic Impairment
Pioglitazone
Compared with healthy controls, subjects with impaired hepatic function (Child-Turcotte-Pugh Grade B/C) have an approximate 45% reduction in pioglitazone and total pioglitazone (pioglitazone, M-III, and M-IV) mean Cmax but no change in the mean AUC values. Therefore, no dosage adjustment in patients with hepatic impairment is required.
There are postmarketing reports of liver failure with pioglitazone and clinical trials have generally excluded patients with serum ALT >2.5 times the upper limit of the reference range. Use ACTOPLUS MET with caution in patients with liver disease [see Warnings and Precautions (5.5)].
Metformin HCl
No pharmacokinetic studies of metformin have been conducted in subjects with hepatic impairment [see Warnings and Precautions (5.5)].
Drug Interaction Studies
Specific pharmacokinetic drug interaction studies with ACTOPLUS MET have not been performed, although such studies have been conducted with the individual pioglitazone and metformin components.
Pioglitazone
Table 18: Effect of Pioglitazone Coadministration on Systemic Exposure of Other Drugs Coadministered Drug
Pioglitazone Dosage
Regimen (mg)*Name and Dose Regimens
Change
in AUC†Change
in Cmax†45 mg
(N = 12)Warfarin‡
Daily loading then maintenance doses
based PT and INR values
Quick's Value = 35 ± 5%R-Warfarin
↓3%
R-Warfarin
↓2%
S-Warfarin
↓1%
S-Warfarin
↑1%
45 mg
(N = 12)Digoxin
0.200 mg twice daily (loading dose) then 0.250 mg daily (maintenance dose, 7 days)
↑15%
↑17%
45 mg daily
for 21 days
(N = 35)Oral Contraceptive
[Ethinyl Estradiol (EE) 0.035 mg plus
Norethindrone (NE) 1 mg] for 21 daysEE
↓11%
EE
↓13%
NE
↑3%
NE
↓7%
45 mg
(N = 23)Fexofenadine
60 mg twice daily for 7 days
↑30%
↑37%
45 mg
(N = 14)Glipizide
5 mg daily for 7 days
↓3%
↓8%
45 mg daily
for 8 days
(N = 16)Metformin
1,000 mg single dose on Day 8
↓3%
↓5%
45 mg
(N = 21)Midazolam
7.5 mg single dose on Day 15
↓26%
↓26%
45 mg
(N = 24)Ranitidine
150 mg twice daily for 7 days
↑1%
↓1%
45 mg daily
for 4 days
(N = 24)Nifedipine ER
30 mg daily for 4 days
↓13%
↓17%
45 mg
(N = 25)Atorvastatin Calcium
80 mg daily for 7 days
↓14%
↓23%
45 mg
(N = 22)Theophylline
400 mg twice daily for 7 days
↑2%
↑5%
Table 19: Effect of Coadministered Drugs on Pioglitazone Systemic Exposure - *
- Daily for 7 days unless otherwise noted.
- †
- Mean ratio (with/without coadministered drug and no change = 1-fold) % change (with/without coadministered drug and no change = 0%); symbols of ↑ and ↓ indicate the exposure increase and decrease, respectively.
- ‡
- The half-life of pioglitazone increased from 8.3 hours to 22.7 hours in the presence of gemfibrozil [see Dosage and Administration (2.3), Drug Interactions (7.1)].
- §
- Indicates duration of concomitant administration with highest twice-daily dose of topiramate from Day 14 onwards over the 22 days of study.
- ¶
- Additional decrease in active metabolites; 60% for M-III and 16% for M-IV.
Coadministered Drug and Dosage Regimen
Pioglitazone
Dose Regimen
(mg)*Change
in AUC†Change
in Cmax†Gemfibrozil 600 mg
twice daily for 2 days
(N = 12)15 mg
single dose↑3.2-fold‡
↑6%
Ketoconazole 200 mg
twice daily for 7 days
(N = 28)45 mg
↑34%
↑14%
Rifampin 600 mg
daily for 5 days
(N = 10)30 mg
single dose↓54%
↓5%
Fexofenadine 60 mg
twice daily for 7 days
(N = 23)45 mg
↑1%
0%
Ranitidine 150 mg
twice daily for 4 days
(N = 23)45 mg
↓13%
↓16%
Nifedipine ER 30 mg
daily for 7 days
(N = 23)45 mg
↑5%
↑4%
Atorvastatin Calcium 80 mg
daily for 7 days
(N = 24)45 mg
↓24%
↓31%
Theophylline 400 mg
twice daily for 7 days
(N = 22)45 mg
↓4%
↓2%
Topiramate 96 mg
twice daily for 7 days§30 mg§
↓15%¶
0%
(N = 26) Metformin HCl
Table 20: Effect of Coadministered Drug on Plasma Metformin Systemic Exposure Coadministered
DrugDose of
Coadministered
Drug*Dose of
Metformin*Geometric Mean Ratio
(ratio with/without coadministered drug)
No effect = 1.00AUC†
Cmax
No dosing adjustments required for the following:
Glyburide
5 mg
500 mg‡
0.98§
0.99§
Furosemide
40 mg
850 mg
1.09§
1.22§
Nifedipine
10 mg
850 mg
1.16
1.21
Propranolol
40 mg
850 mg
0.90
0.94
Ibuprofen
400 mg
850 mg
1.05§
1.07§
Drugs that are eliminated by renal tubular secretion may increase the accumulation of metformin [see Warnings and Precautions (5), Drug Interactions (7)].
Cimetidine
400 mg
850 mg
1.40
1.61
Carbonic anhydrase inhibitors may cause metabolic acidosis [see Warnings and Precautions (5), Drug Interactions (7)].
Topiramate
100 mg¶
500 mg¶
1.25¶
1.17
Table 21: Effect of Metformin on Coadministered Drug Systemic Exposure Coadministered Drug
Dose of Coadministered Drug*
Dose of
Metformin*Geometric Mean Ratio
(ratio with/without coadministered drug)
No effect = 1.00AUC†
Cmax
No dosing adjustments required for the following:
Glyburide
5 mg
500 mg‡
0.78§
0.63§
Furosemide
40 mg
850 mg
0.87§
0.69§
Nifedipine
10 mg
850 mg
1.10‡
1.08
Propranolol
40 mg
850 mg
1.01‡
0.94
Ibuprofen
400 mg
850 mg
0.97¶
1.01¶
Cimetidine
400 mg
850 mg
0.95‡
1.01
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
ACTOPLUS MET
No animal studies have been conducted with ACTOPLUS MET. The following data are based on findings in studies performed with pioglitazone or metformin individually.
Pioglitazone
A two year carcinogenicity study was conducted in male and female rats at oral doses up to 63 mg/kg (approximately 14 times the maximum recommended human oral dose of 45 mg based on mg/m2). Drug-induced tumors were not observed in any organ except for the urinary bladder of male rats. Benign and/or malignant transitional cell neoplasms were observed in male rats at 4 mg/kg/day and above (approximately equal to the maximum recommended human oral dose based on mg/m2). Urinary calculi with subsequent irritation and hyperplasia were postulated as the mechanism for bladder tumors observed in male rats. A two year mechanistic study in male rats utilizing dietary acidification to reduce calculi formation was completed in 2009. Dietary acidification decreased but did not abolish the hyperplastic changes in the bladder. The presence of calculi exacerbated the hyperplastic response to pioglitazone but was not considered the primary cause of the hyperplastic changes.
The relevance to humans of the bladder findings in the male rat cannot be excluded.
A two year carcinogenicity study was also conducted in male and female mice at oral doses up to 100 mg/kg/day (approximately 11 times the maximum recommended human oral dose based on mg/m2). No drug-induced tumors were observed in any organ.
Pioglitazone HCl was not mutagenic in a battery of genetic toxicology studies, including the Ames bacterial assay, a mammalian cell forward gene mutation assay (CHO/HPRT and AS52/XPRT), an in vitro cytogenetics assay using CHL cells, an unscheduled DNA synthesis assay, and an in vivo micronucleus assay.
No adverse effects upon fertility were observed in male and female rats at oral doses up to 40 mg/kg pioglitazone HCl daily prior to and throughout mating and gestation (approximately nine times the maximum recommended human oral dose based on mg/m2).
Metformin HCl
Long-term carcinogenicity studies have been performed in rats (dosing duration of 104 weeks) and mice (dosing duration of 91 weeks) at doses up to and including 900 mg/kg/day and 1500 mg/kg/day, respectively. These doses are both approximately four times a human daily dose of 2000 mg of the metformin component of ACTOPLUS MET based on body surface area comparisons. No evidence of carcinogenicity with metformin was found in either male or female mice. Similarly, there was no tumorigenic potential observed with metformin in male rats. There was, however, an increased incidence of benign stromal uterine polyps in female rats treated with 900 mg/kg/day.
There was no evidence of mutagenic potential of metformin in the following in vitro tests: Ames test (S. typhimurium), gene mutation test (mouse lymphoma cells), or chromosomal aberrations test (human lymphocytes). Results in the in vivo mouse micronucleus test were also negative.
Fertility of male or female rats was unaffected by metformin when administered at doses as high as 600 mg/kg/day, which is approximately three times the maximum recommended human daily dose of the metformin component of ACTOPLUS MET based on body surface area comparisons.
13.2 Animal Toxicology and/or Pharmacology
Heart enlargement has been observed in mice (100 mg/kg), rats (4 mg/kg and above) and dogs (3 mg/kg) treated orally with pioglitazone HCl (approximately 11, one, and two times the maximum recommended human oral dose for mice, rats, and dogs, respectively, based on mg/m2). In a one year rat study, drug-related early death due to apparent heart dysfunction occurred at an oral dose of 160 mg/kg/day (approximately 35 times the maximum recommended human oral dose based on mg/m2). Heart enlargement was seen in a 13 week study in monkeys at oral doses of 8.9 mg/kg and above (approximately four times the maximum recommended human oral dose based on mg/m2), but not in a 52 week study at oral doses up to 32 mg/kg (approximately 13 times the maximum recommended human oral dose based on mg/m2).
-
14 CLINICAL STUDIES
14.1 Patients Who Have Inadequate Glycemic Control with Diet and Exercise Alone
In a 24 week, randomized, double-blind clinical trial, 600 patients with type 2 diabetes mellitus inadequately controlled with diet and exercise alone (mean baseline HbA1c 8.7%) were randomized to ACTOPLUS MET 15/850 mg, pioglitazone 15 mg, or metformin 850 mg twice daily. Statistically significant improvements in HbA1c and fasting plasma glucose (FPG) were observed in patients treated with ACTOPLUS MET compared to either pioglitazone or metformin alone (see Table 22).
Table 22: Glycemic Parameters in 24 Week Study of ACTOPLUS MET in Patients with Type 2 Diabetes Mellitus Inadequately Controlled with Diet and Exercise Parameter
Treatment Group
ACTOPLUS MET 15/850 mg
Twice DailyPioglitazone
15 mg
Twice DailyMetformin
850 mg
Twice DailyHbA1c (%)
N=188
N=162
N=193
Baseline (mean)
8.9
8.7
8.7
Change from Baseline
(adjusted mean*)-1.8
-1.0
-1.0
Difference between ACTOPLUS MET
(adjusted mean*)
95% Confidence Interval0.9†
(0.5, 1.2)0.8†
(0.5, 1.2)% of patients with HbA1c ≤7%
64
47
39
Fasting Plasma Glucose (mg/dL)
N=196
N=176
N=202
Baseline (mean)
177
171
171
Change from Baseline
(adjusted mean*)-40
-22
-25
Difference between ACTOPLUS MET
(adjusted mean*)
95% Confidence Interval18†
(8, 28)15†
(6, 25)14.2 Patients Previously Treated with Metformin
The efficacy and safety of pioglitazone as add-on to metformin therapy have been established in two clinical studies [see Clinical Pharmacology (12.3)].
The two clinical trials testing pioglitazone as add-on to metformin therapy included patients with type 2 diabetes mellitus on any dose of metformin, either alone or in combination with another antidiabetic agent. All other antidiabetic agents were withdrawn at least three weeks prior to starting study treatment.
In the first trial, 328 patients were randomized to receive either 30 mg of pioglitazone or placebo once daily for 16 weeks in addition to their current metformin regimen. Treatment with pioglitazone as add-on to metformin produced statistically significant improvements in HbA1c and FPG at endpoint compared to placebo add-on to metformin (see Table 23).
Table 23: Glycemic Parameters in a 16 Week Placebo-Controlled, Add-on to Metformin Trial Placebo
+ MetforminPioglitazone
30 mg
+ MetforminTotal Population
HbA1c (%)
N=153
N=161
Baseline (mean)
9.8
9.9
Change from baseline (adjusted mean*)
0.2
-0.6
Difference from placebo + metformin (adjusted mean*)
95% Confidence Interval-0.8†
(-1.2, -0.5)Fasting Plasma Glucose (mg/dL)
N=157
N=165
Baseline (mean)
260
254
Change from baseline (adjusted mean*)
-5
-43
Difference from placebo + metformin (adjusted mean*)
95% Confidence Interval-38†
(-49, -26)In the second trial, 827 patients were randomized to receive either 30 mg or 45 mg of pioglitazone once daily for 24 weeks in addition to their current metformin regimen. The mean reduction from baseline at Week 24 in HbA1c was 0.8% for the 30 mg dose and 1.0% for the 45 mg dose (see Table 24). The mean reduction from baseline at Week 24 in FPG was 38 mg/dL for the 30 mg dose and 51 mg/dL for the 45 mg dose.
Table 24: Glycemic Parameters in a 24 Week Add-on to Metformin Study 95% CI = 95% confidence interval. Pioglitazone
30 mg
+ MetforminPioglitazone
45 mg
+ MetforminTotal Population
HbA1c (%)
N=400
N=398
Baseline (mean)
9.9
9.8
Change from baseline
(adjusted mean*)-0.8
-1.0
Difference from 30 mg daily pioglitazone + metformin (adjusted mean*) (95% CI)
-0.2
(-0.5, 0.1)Fasting Plasma Glucose (mg/dL)
N=398
N=399
Baseline (mean)
233
232
Change from baseline
(adjusted mean*)-38
-51
Difference from 30 mg daily pioglitazone + metformin (adjusted mean*) (95% CI)
-12†
(-21, -4)The therapeutic effect of pioglitazone in combination with metformin was observed in patients regardless of the metformin dose.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ACTOPLUS MET is available in 15 mg pioglitazone (as the base)/850 mg metformin HCl tablets as follows:
15 mg/850 mg tablet: white to off-white, oblong, film-coated tablet with "4833M" on one side and "15/850" on the other, available in:
Bottles of 60 NDC 64764-158-60
Bottles of 180 NDC 64764-158-18
Storage
Store at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F) [see USP Controlled Room Temperature]. Keep container tightly closed, and protect from moisture and humidity. -
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
- Congestive Heart Failure: Inform patients of the signs and symptoms of heart failure. Instruct patients who experience an unusually rapid increase in weight or edema, shortness of breath, or other symptoms of heart failure while on ACTOPLUS MET to immediately report these symptoms to their healthcare provider. [see Warnings and Precautions (5.1)].
-
Lactic Acidosis: Explain to patients the risks of lactic acidosis, its symptoms and conditions that predispose to its development, as noted in the Warnings and Precautions (5.2) section. Advise patients to discontinue ACTOPLUS MET immediately and to promptly notify their healthcare professional if unexplained hyperventilation, myalgia, gastrointestinal symptoms, malaise, unusual somnolence, or other nonspecific symptoms occur.
Counsel patients against excessive alcohol intake and inform patients about the importance of regular testing of renal function while receiving ACTOPLUS MET.
Inform patients about the importance of regular testing of renal function and hematologic parameters when receiving treatment with ACTOPLUS MET
Instruct patients to inform their doctor that they are taking ACTOPLUS MET prior to any surgical or radiological procedure, as temporary discontinuation of ACTOPLUS MET may be required until renal function has been confirmed to be normal. - Edema: Inform patients that ACTOPLUS MET use can lead to new-onset or worsening of edema. Instruct patients to immediately report symptoms of rapid weight increase or worsening edema to their healthcare provider [see Warnings and Precautions (5.3)].
- Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues: Inform patients that the risk of hypoglycemia is increased when ACTOPLUS MET is used with insulin or insulin secretagogues (such as a sulfonylurea). Educate patients on the signs and symptoms of hypoglycemia [see Warnings and Precautions (5.4)].
- Hepatic Effects: Instruct patients to promptly stop taking ACTOPLUS MET and seek immediate medical advice if they experience signs or symptoms of liver injury (e.g., unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, or dark urine) [see Warnings and Precautions (5.5)].
- Urinary Bladder Tumors: Advise patients to promptly report any hematuria, dysuria or urinary urgency that develops or increases during treatment as these may be due to bladder cancer [see Warnings and Precautions (5.6)].
- Fractures: Inform female patients about the risk of fractures while taking ACTOPLUS MET. Provide them with information on factors that may contribute to fracture risk [see Warnings and Precautions (5.7)].
- Macular Edema: Educate patients on the signs and symptoms of macular edema and advise them to seek medical attention from an ophthalmologist if they experience symptoms of macular edema [see Warnings and Precautions (5.8)].
- Vitamin B12 Levels: Inform patients about the importance of obtaining regular hematological laboratory monitoring while receiving ACTOPLUS MET [see Warnings and Precautions (5.9)].
- Females of Reproductive Age: Inform female patients that treatment with ACTOPLUS MET may result in an unintended pregnancy in some premenopausal anovulatory females due to its effect on ovulation [see Use in Specific Populations (8.3)]
- Missed Dosage: Instruct patients if a dose is missed, not to double their next dose.
-
SPL UNCLASSIFIED SECTION
Distributed by:
Takeda Pharmaceuticals America, Inc.
Lexington, MA 02421ACTOS and ACTOPLUS MET are trademarks of Takeda Pharmaceutical Company Limited registered with the U.S. Patent and Trademark Office and used under license by Takeda Pharmaceuticals America, Inc.
All other trademarks are the property of their respective owners.
©2024 Takeda Pharmaceuticals America, Inc.
APM001 R17
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration.
APM001 R17
Revised: 06/2024MEDICATION GUIDE
ACTOPLUS MET (ak-TŌ-plus-met)
(pioglitazone and metformin hydrochloride)
tabletsRead this Medication Guide carefully before you start taking ACTOPLUS MET and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. If you have any questions about ACTOPLUS MET, ask your healthcare provider or pharmacist. What is the most important information I should know about ACTOPLUS MET?
ACTOPLUS MET can cause serious side effects, including:
-
Heart failure. Pioglitazone, one of the medicines in ACTOPLUS MET, can cause your body to keep extra fluid (fluid retention), which leads to swelling (edema) and weight gain. Extra body fluid can make some heart problems worse or lead to heart failure. Heart failure means your heart does not pump blood well enough.
Before you start taking ACTOPLUS MET:
Tell your healthcare provider if you have ever had heart failure or have problems with your kidneys
Call your healthcare provider right away if you have any of the following:- increasing shortness of breath or trouble breathing, especially when you lie down
- an unusually fast increase in weight
- swelling or fluid retention, especially in the ankles or legs
- unusual tiredness
These may be symptoms of heart failure.
-
Lactic acidosis. Metformin, one of the medicines in ACTOPLUS MET, can cause a rare but serious condition called lactic acidosis (a buildup of an acid in the blood) that can cause death. Lactic acidosis is a medical emergency and must be treated in the hospital.
Stop taking ACTOPLUS MET and call your healthcare provider right away if you have any of the following symptoms, which could be signs of lactic acidosis:- feel very weak or tired
- have unusual (not normal) muscle pain
- have trouble breathing
- have unusual sleepiness or sleep longer than usual
- have unexplained stomach or intestinal problems with nausea, vomiting, or diarrhea
- feel cold, especially in your arms and legs
- feel dizzy or lightheaded
- have a slow or irregular heartbeat
Most people who have had lactic acidosis with metformin have other things that, combined with the metformin, led to the lactic acidosis. Tell your healthcare provider if you have any of the following, because you have a higher chance for getting lactic acidosis with ACTOPLUS MET if you: - have severe kidney problems or your kidneys are affected by certain x-ray tests that use injectable dye.
- have liver problems
- drink alcohol very often, or drink a lot of alcohol in short-term ("binge" drinking)
- get dehydrated (lose a large amount of body fluids). This can happen if you are sick with a fever, vomiting, or diarrhea. Dehydration can also happen when you sweat a lot with activity or exercise and do not drink enough fluids
- have surgery
- have a heart attack, severe infection, or stroke
- are 65 years of age or older
The best way to keep from having a problem with lactic acidosis from metformin is to tell your healthcare provider if you have any of the problems in the list above. Your healthcare provider may decide to stop your ACTOPLUS MET for a while if you have any of these things.
ACTOPLUS MET can have other serious side effects. See “What are the possible side effects of ACTOPLUS MET?”.
What is ACTOPLUS MET?
ACTOPLUS MET is a prescription medicine that contains 2 diabetes medicines, pioglitazone (ACTOS) and metformin hydrochloride (GLUCOPHAGE). ACTOPLUS MET is used along with diet and exercise to improve blood sugar (glucose) control in adults with type 2 diabetes.
ACTOPLUS MET is not for people with type 1 diabetes.
ACTOPLUS MET is not for people with diabetic ketoacidosis (increased ketones in your blood or urine).
It is not known if ACTOPLUS MET is safe and effective in children under the age of 18. ACTOPLUS MET is not recommended for use in children.
Who should not take ACTOPLUS MET?
See “What is the most important information I should know about ACTOPLUS MET?”.
Do not take ACTOPLUS MET if you:
- have severe heart failure
- have severe kidney problems
- have a condition called acute or chronic metabolic acidosis, including diabetic ketoacidosis.
- are allergic to pioglitazone, metformin, or any of the ingredients in ACTOPLUS MET or have had a serious allergic (hypersensitivity) reaction to pioglitazone or metformin. See the end of this Medication Guide for a complete list of ingredients in ACTOPLUS MET. Symptoms of a serious allergic reaction to ACTOPLUS MET may include:
- swelling of your face, lips, throat and other areas on your skin
- raised, red areas on your skin (hives)
- difficulty with swallowing or breathing
- skin rash, itching, flaking or peeling
If you have these symptoms, stop taking ACTOPLUS MET and contact your healthcare provider or go to the nearest hospital emergency room right away.
Tell your healthcare provider before taking ACTOPLUS MET if you have any of these conditions.
What should I tell my healthcare provider before taking ACTOPLUS MET?
Before you take ACTOPLUS MET, tell your healthcare provider if you:
- have heart failure
- have kidney or liver problems
- are going to have dye injected into a vein for an x-ray, CAT scan, heart study, or other type of scanning
- will be undergoing a surgical procedure
- drink a lot of alcohol (all the time or short binge drinking)
- have type 1 ("juvenile") diabetes or had diabetic ketoacidosis
- have a type of diabetic eye disease that causes swelling in the back of the eye (macular edema)
- have low levels of vitamin B12 in your blood
- have or have had cancer of the bladder
- are pregnant or plan to become pregnant. It is not known if ACTOPLUS MET can harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant about the best way to control your blood glucose levels while pregnant
-
are a woman who has not gone through menopause (premenopausal), who does not have periods regularly or at all. ACTOPLUS MET may increase your chance of becoming pregnant.
Talk to your healthcare provider about birth control choices while taking ACTOPLUS MET. Tell your healthcare provider right away if you become pregnant while taking ACTOPLUS MET - are breastfeeding or plan to breastfeed. It is not known if ACTOPLUS MET passes into your milk and if it can harm your baby. Talk to your healthcare provider about the best way to control your blood glucose levels while breastfeeding
Tell your healthcare provider about all the medicines you take, including prescription and over the counter medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of your medicines and show it to your healthcare provider and pharmacist before you start a new medicine. They will tell you if it is okay to take ACTOPLUS MET with other medicines.
ACTOPLUS MET may affect the way other medicines work, and other medicines may affect how ACTOPLUS MET works. Contact your healthcare provider before you start or stop other types of medicines.
How should I take ACTOPLUS MET?
- Take ACTOPLUS MET exactly as your healthcare provider tells you to take it
- Your healthcare provider may need to change your dose of ACTOPLUS MET. Do not change your ACTOPLUS MET dose unless your healthcare provider tells you to
- Take ACTOPLUS MET with meals to lower your chance of an upset stomach
- If you miss a dose of ACTOPLUS MET, take your next dose as prescribed unless your healthcare provider tells you differently. Do not take two doses at one time the next day
- If you take too much ACTOPLUS MET, call your healthcare provider or go to the nearest hospital emergency room right away
- If your body is under stress such as from a fever, infection, accident, or surgery, the dose of your diabetes medicines may need to be changed. Call your healthcare provider right away
- Stay on your diet and exercise programs and test your blood sugar regularly while taking ACTOPLUS MET
- Your healthcare provider should do certain blood tests before you start and while you take ACTOPLUS MET
- Your healthcare provider should also do hemoglobin A1C testing to check how well your blood sugar is controlled with ACTOPLUS MET
- Your healthcare provider should check your eyes regularly while you take ACTOPLUS MET
What are the possible side effects of ACTOPLUS MET?
ACTOPLUS MET may cause serious side effects, including:
- See “What is the most important information I should know about ACTOPLUS MET?”.
-
Low blood sugar (hypoglycemia). If you take ACTOPLUS MET with another medicine that can cause low blood sugar, such as a sulfonylurea or insulin, your risk of getting low blood sugar is higher. The dose of your sulfonylurea medicine or insulin may need to be lowered while you take ACTOPLUS MET. Signs and symptoms of low blood sugar may include:
- shaking or feeling jittery ∘ sweating ∘ fast heartbeat
- change in vision ∘ hunger ∘ headache
- change in mood ∘ confusion ∘ dizziness
-
Liver problems. Call your healthcare provider right away or go to the nearest hospital emergency room if you have unexplained symptoms such as:
- nausea or vomiting
- stomach pain
- unusual or unexplained tiredness
- loss of appetite
- dark urine
- yellowing of your skin or the whites of your eyes
-
Bladder tumors. There may be an increased chance of having bladder cancer when you take ACTOPLUS MET. You should not take ACTOPLUS MET if you are receiving treatment for bladder cancer. Tell your healthcare provider right away if you have any of the following symptoms of bladder cancer:
- blood or a red color in your urine
- an increased need to urinate
- pain while you urinate
- Broken bones (fractures). Usually in the hand, upper arm, or foot in women. Talk to your healthcare provider for advice on how to keep your bones healthy
- Diabetic eye disease with swelling in the back of the eye (macular edema). Tell your healthcare provider right away if you have any changes in your vision. Your healthcare provider should check your eyes regularly
- Release of an egg from an ovary in a woman (ovulation) leading to pregnancy. Ovulation may happen when premenopausal women who do not have regular monthly periods take ACTOPLUS MET. This can increase your chance of getting pregnant.
-
Low vitamin B12 (vitamin B12 deficiency). Using metformin, one of the medicines in ACTOPLUS MET for long periods of time may cause a decrease in the amount of vitamin B12 in your blood, especially if you have had low vitamin B12 levels before. Your healthcare provider may do blood tests to check your vitamin B12 levels. The most common side effects of ACTOPLUS MET include:
- cold-like symptoms (upper respiratory tract infection)
- swelling (edema)
- diarrhea
- headache
- increased weight
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the side effects of ACTOPLUS MET. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ACTOPLUS MET?
- Store ACTOPLUS MET at 68°F to 77°F (20°C to 25°C).
- Keep ACTOPLUS MET in the original container and protect from light.
- Keep the ACTOPLUS MET bottle tightly closed and keep tablets dry.
Keep ACTOPLUS MET and all medicines out of the reach of children.
General information about the safe and effective use of ACTOPLUS MET
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ACTOPLUS MET for a condition for which it was not prescribed. Do not give ACTOPLUS MET to other people, even if they have the same symptoms you have. It may harm them.
You can ask your healthcare provider or pharmacist for information about ACTOPLUS MET that is written for health professionals.
What are the ingredients in ACTOPLUS MET?
Active Ingredients: pioglitazone hydrochloride and metformin hydrochloride
Inactive Ingredients: povidone, microcrystalline cellulose, croscarmellose sodium, magnesium stearate, hypromellose 2910, polyethylene glycol 8000, titanium dioxide, and talc
ACTOS and ACTOPLUS MET are trademarks of Takeda Pharmaceutical Company Limited registered with the U.S. Patent and Trademark Office and used under license by Takeda Pharmaceuticals America, Inc.
Distributed by:
Takeda Pharmaceuticals America, Inc.
Lexington, MA 02421©2024 Takeda Pharmaceuticals America, Inc.
For more information, go to www.actoplusmet.com or call 1-877-825-3327.
-
Heart failure. Pioglitazone, one of the medicines in ACTOPLUS MET, can cause your body to keep extra fluid (fluid retention), which leads to swelling (edema) and weight gain. Extra body fluid can make some heart problems worse or lead to heart failure. Heart failure means your heart does not pump blood well enough.
-
PRINCIPAL DISPLAY PANEL - 15 mg/850 mg Tablet Bottle Label
NDC 64764-158-60
60 Tabletsactoplus met
pioglitazone 15 mg and
metformin HCl 850 mg tabletsEach film-coated tablet contains
pioglitazone hydrochloride
equivalent to 15 mg pioglitazone
and 850 mg metformin HCl.Dispense with Medication Guide
available in package insert or at
www.actoplusmet.comTakeda
Rx Only
-
INGREDIENTS AND APPEARANCE
ACTOPLUS MET
pioglitazone and metformin hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:64764-158 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PIOGLITAZONE HYDROCHLORIDE (UNII: JQT35NPK6C) (pioglitazone - UNII:X4OV71U42S) pioglitazone 15 mg metformin hydrochloride (UNII: 786Z46389E) (metformin - UNII:9100L32L2N) metformin hydrochloride 850 mg Inactive Ingredients Ingredient Name Strength POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) microcrystalline cellulose (UNII: OP1R32D61U) croscarmellose sodium (UNII: M28OL1HH48) magnesium stearate (UNII: 70097M6I30) hypromellose 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) polyethylene glycol 8000 (UNII: Q662QK8M3B) titanium dioxide (UNII: 15FIX9V2JP) talc (UNII: 7SEV7J4R1U) Product Characteristics Color WHITE (white to off-white) Score no score Shape OVAL (oblong) Size 18mm Flavor Imprint Code 4833M;15;850 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:64764-158-60 60 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 08/29/2005 2 NDC:64764-158-18 180 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 08/29/2005 3 NDC:64764-158-41 4 in 1 TRAY 08/29/2005 3 1 in 1 CARTON 3 7 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021842 08/29/2005 Labeler - Takeda Pharmaceuticals America, Inc. (039997266) Establishment Name Address ID/FEI Business Operations Daito Pharmaceutical Co., Ltd 691240774 ANALYSIS(64764-158) , MANUFACTURE(64764-158) Establishment Name Address ID/FEI Business Operations Farmhispania S.A. 462038145 API MANUFACTURE(64764-158) Establishment Name Address ID/FEI Business Operations Juzen Chemical Corporation 691036974 API MANUFACTURE(64764-158) Establishment Name Address ID/FEI Business Operations ZACH SYSTEM S.A. 552044943 API MANUFACTURE(64764-158) Establishment Name Address ID/FEI Business Operations AndersonBrecon Inc. 053217022 LABEL(64764-158) , PACK(64764-158) Establishment Name Address ID/FEI Business Operations Pace Analytical Life Sciences, LLC 797903197 ANALYSIS(64764-158) Establishment Name Address ID/FEI Business Operations Takeda Ireland Ltd. 986017670 MANUFACTURE(64764-158)