Label: ANGELIQ- drospirenone and estradiol tablet, film coated
-
NDC Code(s):
50419-482-01,
50419-482-03,
50419-482-71,
50419-482-72, view more50419-483-01, 50419-483-03, 50419-483-71, 50419-483-72
- Packager: Bayer HealthCare Pharmaceuticals Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated December 8, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ANGELIQ safely and effectively. See full prescribing information for ANGELIQ.
ANGELIQ (drospirenone and estradiol) tablets, for oral use
Initial U.S. Approval: 2005WARNING: CARDIOVASCULAR DISORDERS, PROBABLE DEMENTIA BREAST CANCER, and ENDOMETRIAL CANCER
See full prescribing information for complete boxed warning
Estrogen Plus Progestin Therapy
- •
- The Women’s Health Initiative (WHI) estrogen plus progestin substudy reported increased risks of pulmonary embolism (PE), deep vein thrombosis (DVT), stroke, and myocardial infarction (MI) (5.1)
- •
- The WHI estrogen plus progestin substudy reported increased risks of invasive breast cancer (5.2)
- •
- The WHI Memory Study (WHIMS) estrogen plus progestin ancillary study of WHI reported an increased risk of probable dementia in postmenopausal women 65 years of age and older (5.4)
- •
- Do not use estrogen plus progestogen therapy for the prevention of cardiovascular disease or dementia (5.1), 5.4)
- Estrogen-Alone Therapy
- •
- There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens (5.3)
- •
- The WHI estrogen-alone substudy reported increased risks of stroke and DVT (5.1)
- •
- The WHIMS estrogen-alone ancillary study of WHI reported an increased risk of probable dementia in postmenopausal women 65 years of age and older (5.4)
Do not use estrogen-alone therapy for the prevention of cardiovascular disease or dementia (5.1), 5.4)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Angeliq is a combination of an estrogen and progestin indicated in a woman with a uterus for the treatment of:
- •
- Moderate to severe vasomotor symptoms due to menopause. (1.1)
- •
- Moderate to severe vulvar and vaginal atrophy symptoms due to menopause. (1.2)
- Limitation of Use
- When prescribing solely for the treatment of moderate to severe symptoms of vulvar and vaginal atrophy, first consider the use of topical vaginal products.
Use estrogen, alone or in combination with a progestogen, at the lowest effective dose and the shortest duration consistent with treatment goals and risks for the individual woman. Re-evaluate postmenopausal women periodically as clinically appropriate to determine whether treatment is still necessary.
DOSAGE AND ADMINISTRATION
- •
- Start therapy with Angeliq 0.25 mg drospirenone (DRSP)/0.5 mg estradiol (E2) once daily for the treatment of moderate to severe vasomotor symptoms due to menopause. Dosage adjustment should be guided by the clinical response (2.1)
- •
- Start therapy with Angeliq 0.5 mg DRSP/1 mg E2 once daily for the treatment of moderate to severe vulvar and vaginal atrophy due to menopause (2.2)
DOSAGE FORMS AND STRENGTHS
- •
- Tablet: 0.25 mg DRSP/0.5 mg E2 and 0.5 mg DRSP/1 mg E2 (3)
CONTRAINDICATIONS
- •
- Undiagnosed abnormal genital bleeding (4, 5.3)
- •
- Breast cancer or a history of breast cancer (4, 5.3)
- •
- Estrogen-dependent neoplasia (4, 5.3)
- •
- Active DVT, PE, or a history of these conditions (4, 5.1)
- •
- Active arterial thromboembolic disease (for example, stroke and MI), or history of these conditions (4, 5.1)
- •
- Renal impairment (4, 5.2)
- •
- Hepatic impairment or disease (4, 5.2)
- •
- Adrenal insufficiency (4, 5.2)
- •
- Protein C, protein S, or antithrombin deficiency, or other known thrombophilic disorders (4)
- •
- Known anaphylactic reaction, angioedema, or hypersensitivity to Angeliq (4, 5.16)
WARNINGS AND PRECAUTIONS
- •
- Do not use with conditions that predispose to hyperkalemia (5.2
- •
- Estrogens increase the risk of gallbladder disease (5.5)
- •
- Discontinue estrogen if severe hypercalcemia, loss of vision, severe hypertriglyceridemia or cholestatic jaundice occurs (5.6, 5.7, 5.9, 5.10)
- •
- Monitor thyroid function in women on thyroid hormone replacement therapy (5.11, 5.19)
ADVERSE REACTIONS
The most common adverse reactions with Angeliq that occurred in at least 1% of users in clinical trials are: gastrointestinal and abdominal pain, female genital tract bleeding, breast pain and discomfort, and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bayer HealthCare Pharmaceuticals Inc. at 1-888-842-2937 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CARDIOVASCULAR DISORDERS, PROBABLE DEMENTIA,
BREAST CANCER, and ENDOMETRIAL CANCER1 INDICATIONS AND USAGE
1.1 Treatment of Moderate to Severe Vasomotor Symptoms due to Menopause
1.2 Treatment of Moderate to Severe Symptoms of Vulvar and Vaginal Atrophy due to Menopause
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Moderate to Severe Vasomotor Symptoms due to Menopause
2.2 Treatment of Moderate to Severe Symptoms of Vulvar and Vaginal Atrophy due to Menopause
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Disorders
5.2 Hyperkalemia
5.3 Malignant Neoplasms
5.4 Probable Dementia
5.5 Gallbladder Disease
5.6 Hypercalcemia
5.7 Visual Abnormalities
5.8 Elevated Blood Pressure
5.9 Exacerbation of Hypertriglyceridemia
5.10 Hepatic Impairment and/or Past History of Cholestatic Jaundice
5.11 Exacerbation of Hypothyroidism
5.12 Fluid Retention
5.13 Hypocalcemia
5.14 Hyponatremia
5.15 Exacerbation of Endometriosis
5.16 Hereditary Angioedema
5.17 Exacerbation of Other Conditions
5.18 Laboratory Tests
5.19 Interference with Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Metabolic Interactions
7.2 Interaction with Alcohol
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Adrenal Insufficiency
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Effects on Vasomotor Symptoms in Postmenopausal Women
14.2 Effects on Endometrium in Postmenopausal Women
14.3 Effects on Uterine Bleeding or Spotting in Postmenopausal Women
14.4 Women's Health Initiative Studies
14.5 Women's Health Initiative Memory Study
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CARDIOVASCULAR DISORDERS, PROBABLE DEMENTIA,
BREAST CANCER, and ENDOMETRIAL CANCEREstrogen Plus Progestin Therapy
Cardiovascular Disorders and Probable Dementia
The Women's Health Initiative (WHI) estrogen plus progestin substudy reported increased risks of pulmonary embolism (PE), deep vein thrombosis (DVT), stroke, and myocardial infarction (MI) in postmenopausal women (50 to 79 years of age) during 5.6 years of treatment with daily oral conjugated estrogens (CE) [0.625 mg] combined with medroxyprogesterone acetate (MPA) [2.5 mg], relative to placebo [see Warnings and Precautions (5.1), and Clinical Studies (14.5)].
The WHI Memory Study (WHIMS) estrogen plus progestin ancillary study of WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years of age and older during 4 years of treatment with daily CE (0.625 mg) combined with MPA (2.5 mg), relative to placebo. It is unknown whether this finding applies to younger postmenopausal women [see Warnings and Precautions (5.4), Use in Specific Populations (8.5), and Clinical Studies (14.5)].
Do not use estrogen plus progestogen therapy for the prevention of cardiovascular disease or dementia [see Warnings and Precautions (5.1, 5.4), Clinical Studies (14.4), 14.5)].
Breast Cancer
The WHI estrogen plus progestin substudy demonstrated an increased risk of invasive breast cancer [see Warnings and Precautions (5.3), and Clinical Studies (14.4)].
Only daily oral 0.625 mg CE and 2.5 mg MPA were studied in the estrogen plus progestin substudy of WHI. Therefore, the relevance of the WHI findings regarding adverse cardiovascular events, dementia and breast cancer to lower CE plus other MPA doses, other routes of administration, or other estrogen plus progestin products is not known. Without such data, it is not possible to definitively exclude these risks or determine the extent of these risks for other products. Discuss with your patient the benefits and risks of estrogen plus progestin therapy, taking into account her individual risk profile.
Prescribe estrogens with or without progestogens at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
Estrogen-Alone Therapy
Endometrial Cancer
There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens. Adding a progestogen to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Perform adequate diagnostic measures, including directed or random endometrial sampling when indicated, to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding [see Warnings and Precautions (5.3)].
Cardiovascular Disorders and Probable Dementia
The WHI estrogen-alone substudy reported increased risks of stroke and DVT in postmenopausal women (50 to 79 years of age) during 7.1 years of treatment with daily oral CE (0.625 mg)-alone, relative to placebo [see Warnings and Precautions (5.1), and Clinical Studies (14.5)].
The WHIMS estrogen-alone ancillary study of WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years of age and older during 5.2 years of treatment with daily CE (0.625 mg)-alone, relative to placebo. It is unknown whether this finding applies to younger postmenopausal women [see Warnings and Precautions (5.4), Use in Specific Populations (8.5), and Clinical Studies (14.5)].
Do not use estrogen-alone therapy for the prevention of cardiovascular disease or dementia [see Warnings and Precautions (5.1, 5.4) and Clinical Studies (14.4, 14.5)].
Only daily oral 0.625 mg CE was studied in the estrogen-alone substudy of the WHI. Therefore, the relevance of the WHI findings regarding adverse cardiovascular events and dementia to lower CE doses, other routes of administration, or other estrogen-alone products is not known. Without such data, it is not possible to definitively exclude these risks or determine the extent of these risks for other products. Discuss with your patient the benefits and risks of estrogen-alone therapy, taking into account her individual risk profile.
Prescribe estrogens with or without progestogens at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
-
1 INDICATIONS AND USAGE
1.1 Treatment of Moderate to Severe Vasomotor Symptoms due to Menopause
- •
- Angeliq 0.25 mg drospirenone (DRSP)/0.5 mg estradiol (E2) is indicated for the treatment of moderate to severe vasomotor symptoms due to menopause in a woman with a uterus.
- •
- Angeliq 0.5 mg DRSP/1 mg E2 is indicated for the treatment of moderate to severe symptoms of vulvar and vaginal atrophy due to menopause in a woman with a uterus.
-
2 DOSAGE AND ADMINISTRATION
Each pack of Angeliq covers 28 days of treatment. Treatment is continuous, which means that the next pack follows immediately without a break. The tablets are to be swallowed whole with some liquid irrespective of food intake and should preferably be taken at the same time every day. In case a tablet is forgotten, it should be taken as soon as possible. If more than 24 hours have elapsed, the missed tablet should not be taken. If several tablets are forgotten, bleeding may occur.
Women who do not take estrogens or women who change from a continuous combination product may start treatment at any time. Women changing from a continuous sequential or cyclic hormone therapy (HT) should complete the current cycle of therapy before initiating Angeliq therapy.
2.1 Treatment of Moderate to Severe Vasomotor Symptoms due to Menopause
One 0.25 mg DRSP/0.5 mg E2 tablet or one Angeliq 0.5 mg DRSP/1 mg E2 tablet taken by mouth once daily.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Angeliq is contraindicated in women with any of the following conditions:
- •
- Undiagnosed abnormal genital bleeding [see Warnings and Precautions (5.3)].
- •
- Breast cancer or a history of breast cancer [see Warnings and Precautions (5.3)].
- •
- Estrogen-dependent neoplasia [see Warnings and Precautions (5.3)].
- •
- Active DVT, PE or history of these conditions [see Warnings and Precautions (5.1)].
- •
- Active arterial thromboembolic disease (for example, stroke and MI) or history of these conditions [see Warnings and Precautions (5.1)].
- •
- Renal Impairment [see Warnings and Precautions (5.2), Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
- •
- Hepatic impairment or disease [see Warnings and Precautions (5.10), Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
- •
- Adrenal insufficiency [see Warnings and Precautions (5.2)].
- •
- Protein C, protein S, or antithrombin deficiency, or other known thrombophilic disorders
- •
- Known anaphylactic reaction, angioedema, or hypersensitivity to Angeliq or any of its ingredients [see Adverse Reactions (6.2)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Disorders
Increased risks of PE, DVT, stroke, and MI are reported with estrogen plus progestin therapy. Increased risks of stroke and DVT are reported with estrogen-alone therapy. Immediately discontinue estrogen with or without progestogen therapy if any of these occur or are suspected.
Manage appropriately any risk factors for arterial vascular disease (for example, hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and/or obesity) and/or venous thromboembolism (VTE) [for example, personal history or family history of VTE, obesity, systemic lupus erythematosus].
Stroke
The WHI estrogen plus progestin substudy reported a statistically significant increased risk of stroke in women 50 to 79 years of age receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women in the same age group receiving placebo (33 versus 25 strokes per 10,000 women years, respectively) [see Clinical Studies (14.4)]. The increase in risk was demonstrated after the first year and persisted.1 Immediately discontinue estrogen with or without progestogen therapy if a stroke occurs or is suspected.
The WHI estrogen-alone substudy reported a statistically significant increased risk of stroke in women 50 to 79 years of age receiving daily CE (0.625 mg)-alone compared to women in the same age group receiving placebo (45 versus 33 strokes per 10,000 women-years). The increase in risk was demonstrated in year one and persisted 1[see Clinical Studies (14.4)]. Immediately discontinue estrogen-alone therapy if a stroke occurs or is suspected.
Subgroup analyses of women 50 to 59 years of age suggest no increased risk of stroke for those women receiving CE (0.625 mg)-alone versus those receiving placebo (18 versus 21 per 10,000 women-years).1
Coronary Heart Disease
The WHI estrogen plus progestin substudy reported an increased risk (not statistically significant) of coronary heart disease (CHD) events (defined as nonfatal MI, silent MI, or CHD death) in those women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women receiving placebo (41 versus 34 per 10,000 women-years).1 An increase in relative risk was demonstrated in year 1, and a trend toward decreasing relative risk was reported in years 2 through 5 [see Clinical Studies (14.4)].
The WHI estrogen-alone substudy reported no overall effect on CHD events in women receiving estrogen-alone compared to placebo2[see Clinical Studies (14.4)].
Subgroup analyses of women 50 to 59 years of age, who were less than 10 years since menopause, suggest a reduction (not statistically significant) in CHD events in those women receiving daily CE (0.625 mg)-alone compared to placebo (8 versus 16 per 10,000 women-years).1
In postmenopausal women with documented heart disease (n=2,763), average 66.7 years of age, in a controlled clinical trial of secondary prevention of cardiovascular disease (Heart and Estrogen/Progestin Replacement Study; HERS), treatment with daily CE (0.625 mg) plus MPA (2.5 mg) demonstrated no cardiovascular benefit. During an average follow-up of 4.1 years, treatment with CE plus MPA did not reduce the overall rate of CHD events in postmenopausal women with established CHD. There were more CHD events in the CE plus MPA-treated group than in the placebo group in year 1, but not during the subsequent years. Two thousand, three hundred and twenty-one (2,321) women from the original HERS trial agreed to participate in an open label extension of HERS, HERS II. Average follow-up in HERS II was an additional 2.7 years, for a total of 6.8 years overall. Rates of CHD events were comparable among women in the CE plus MPA group and the placebo group in HERS, HERS II, and overall.
Venous Thromboembolism
The WHI estrogen plus progestin substudy reported a statistically significant 2-fold greater rate of VTE (DVT and PE) in women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women receiving placebo (35 versus 17 per 10,000 women-years). Statistically significant increases in risk for both DVT (26 versus 13 per 10,000 women-years) and PE (18 versus 8 per 10,000 women-years) were also demonstrated. The increase in VTE risk was demonstrated during the first year and persisted3 [see Clinical Studies (14.4)]. Immediately discontinue estrogen plus progestogen therapy if a VTE occurs or is suspected.
In the WHI estrogen-alone substudy, the risk of VTE was increased for women receiving daily CE (0.625 mg)-alone compared to placebo (30 versus 22 per 10,000 women-years), although only the increased risk of DVT reached statistical significance (23 versus 15 per 10,000 women-years). The increase in VTE risk was demonstrated during the first 2 years4 [see Clinical Studies (14.4)]. Immediately discontinue estrogen-alone therapy if a VTE occurs or is suspected.
If feasible, discontinue estrogens at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism, or during periods of prolonged immobilization.
5.2 Hyperkalemia
Angeliq contains the progestin DRSP that has antialdosterone activity, including the potential for hyperkalemia in high-risk patients. Angeliq is contraindicated in patients with conditions that predispose to hyperkalemia (renal impairment, hepatic impairment, and adrenal insufficiency).
Use caution when prescribing Angeliq to women who regularly take other medications that can increase potassium, such as non-steroidal anti-inflammatory drugs (NSAIDs), potassium-sparing diuretics, potassium supplements, angiotensin converting enzyme (ACE) inhibitors, angiotensin-II receptor antagonists, heparin and aldosterone antagonists. Consider monitoring serum potassium concentrations during the first month of dosing in high-risk patients who take strong CYP3A4 inhibitors long-term and concomitantly. Strong CYP3A4 inhibitors include azole antifungals (for example, ketoconazole, itraconazole, voriconazole), human immunodeficiency virus (HIV)/hepatitis C virus (HCV) protease inhibitors (for example, indinavir, boceprevir), and clarithromycin [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
5.3 Malignant Neoplasms
Breast Cancer
After a mean follow-up of 5.6 years, the WHI substudy of daily CE (0.625 mg) plus MPA (2.5 mg) reported an increased risk of invasive breast cancer in women who took daily CE plus MPA compared to placebo. In this substudy, prior use of estrogen-alone or estrogen plus progestin therapy was reported by 26 percent of the women. The relative risk of invasive breast cancer was 1.24 and the absolute risk was 41 versus 33 cases per 10,000 women-years, for CE plus MPA compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86 and the absolute risk was 46 versus 25 cases per 10,000 women-years for CE plus MPA compared with placebo. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09 and the absolute risk was 40 versus 36 cases per 10,000 women-years for CE plus MPA compared with placebo. In the same substudy, invasive breast cancers were larger, were more likely to be node positive, and were diagnosed at a more advanced stage in the CE (0.625 mg) plus MPA (2.5 mg) group compared with the placebo group. Metastatic disease was rare, with no apparent difference between the two groups. Other prognostic factors, such as histologic subtype, grade and hormone receptor status did not differ between the groups5 [see Clinical Studies (14.4)].
The WHI substudy of daily CE (0.625 mg)-alone provided information about breast cancer in estrogen-alone users. In the WHI estrogen-alone substudy, after an average follow-up of 7.1 years, daily CE (0.625 mg)-alone was not associated with an increased risk of invasive breast cancer [relative risk (RR) 0.80]6 compared to placebo [see Clinical Studies (14.4)].
Consistent with the WHI clinical trial, observational studies have also reported an increased risk of breast cancer with estrogen plus progestin therapy, and a smaller increase in the risk for breast cancer with estrogen-alone therapy, after several years of use. One large meta-analysis of prospective cohort studies reported increased risks that were dependent upon duration of use and could last up to >10 years after discontinuation of estrogen plus progestin therapy and estrogen-alone therapy. Extension of the WHI trials also demonstrated increased breast cancer risk associated with estrogen plus progestin therapy. Observational studies also suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen plus progestin therapy as compared to estrogen-alone therapy. These studies have not generally found significant variation in the risk of breast cancer among different estrogen plus progestin combinations, doses, or routes of administration.
The use of estrogen-alone and estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation.
All women should receive yearly breast examinations by a healthcare provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.
Endometrial Cancer
An increased risk of endometrial cancer has been reported with the use of unopposed estrogen therapy in a woman with a uterus. The reported endometrial cancer risk among unopposed estrogen users is about 2- to 12-fold greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than 1 year. The greatest risk appears associated with prolonged use, with increased risks of 15- to 24-fold for 5 to 10 years or more. This risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued.
Clinical surveillance of all women using estrogen-alone or estrogen plus progestin therapy is important. Perform adequate diagnostic measures, including directed or random endometrial sampling when indicated, to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding with unknown etiology.
There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Adding a progestogen to estrogen therapy in postmenopausal women has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer.
Ovarian Cancer
The CE plus MPA substudy of WHI reported that estrogen plus progestin increased the risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for CE plus MPA versus placebo was 1.58 (95 percent CI 0.77-3.24) but was not statistically significant. The absolute risk for CE plus MPA versus placebo was 4 versus 3 cases per 10,000 women-years.7
A meta-analysis of 17 prospective and 35 retrospective epidemiology studies found that women who used hormonal therapy for menopausal symptoms had an increased risk for ovarian cancer. The primary analysis, using case-control comparisons, included 12,110 cancer cases from the 17 prospective studies. The relative risks associated with current use of hormonal therapy was 1.41 (95% confidence interval [CI] 1.32 to 1.50); there was no difference in the risk estimates by duration of the exposure (less than 5 years [median of 3 years] vs. greater than 5 years [median of 10 years] of use before the cancer diagnosis). The relative risk associated with combined current and recent use (discontinued use within 5 years before cancer diagnosis) was 1.37 (95% CI 1.27 to 1.48), and the elevated risk was significant for both estrogen-alone and estrogen plus progestin products. The exact duration of hormone therapy use associated with an increased risk of ovarian cancer, however, is unknown.
5.4 Probable Dementia
In the WHI Memory Study (WHIMS) estrogen plus progestin ancillary study, a population of 4,532 postmenopausal women 65 to 79 years of age was randomized to daily CE (0.625 mg) plus MPA (2.5 mg) or placebo. After an average follow-up of 4 years, 40 women in the CE plus MPA group and 21 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE plus MPA versus placebo was 2.05 (95 percent CI, 1.21-3.48). The absolute risk of probable dementia for CE plus MPA versus placebo was 45 versus 22 cases per 10,000 women-years8 [see Use in Specific Populations (8.5), and Clinical Studies (14.5)].
In the WHIMS estrogen-alone ancillary study, a population of 2,947 hysterectomized women 65 to 79 years of age was randomized to daily CE (0.625 mg)-alone or placebo. After an average follow-up of 5.2 years, 28 women in the estrogen-alone group and 19 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE-alone versus placebo was 1.49 (95 percent CI, 0.83-2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years8 [see Use in Specific Populations (8.5) and Clinical Studies (14.5)].
When data from the two populations in the WHIMS estrogen-alone and estrogen plus progestin ancillary studies were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95 percent CI 1.19-2.60). Since both ancillary studies were conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women8 [see Use in Specific Populations (8.5) and Clinical Studies (14.5)].
5.5 Gallbladder Disease
A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal women receiving estrogens has been reported.
5.6 Hypercalcemia
Estrogen administration may lead to severe hypercalcemia in women with breast cancer and bone metastases. Discontinue estrogen plus progestin, including Angeliq if hypercalcemia occurs, and take appropriate measures to reduce the serum calcium concentration.
5.7 Visual Abnormalities
Retinal vascular thrombosis has been reported in women receiving estrogens. Discontinue Angeliq pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia, or migraine. Permanently discontinue estrogen plus progestin, including Angeliq, if examination reveals papilledema or retinal vascular lesions.
5.8 Elevated Blood Pressure
In a small number of case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogen therapy on blood pressure was not seen.
5.9 Exacerbation of Hypertriglyceridemia
In women with pre-existing hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis. Discontinuation Angeliq if pancreatitis occurs.
5.10 Hepatic Impairment and/or Past History of Cholestatic Jaundice
Estrogens may be poorly metabolized in women with hepatic impairment. Exercise caution in any woman with a history of cholestatic jaundice associated with past estrogen use or with pregnancy. In the case of recurrence of cholestatic jaundice, discontinue Angeliq.
The clearance of drospirenone was decreased in patients with moderate hepatic impairment.
5.11 Exacerbation of Hypothyroidism
Estrogen administration leads to increased thyroid-binding globulin (TBG) concentrations. Women with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T4 and T3 serum concentrations in the normal range. Women dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. Monitor thyroid function in these women during treatment with Angeliq to maintain their free thyroid hormone concentrations in an acceptable range.
5.12 Fluid Retention
Estrogens plus progestogens may cause some degree of fluid retention. Monitor any woman with a condition(s) that might predispose her to fluid retention, such as a cardiac or renal impairment. Discontinue estrogen plus progestogen therapy, including Angeliq, with evidence of medically concerning fluid retention.
5.13 Hypocalcemia
Estrogen-induced hypocalcemia may occur in women with hypoparathyroidism. Consider whether the benefits of estrogen therapy, including Angeliq, outweigh the risks in such women.
5.14 Hyponatremia
As an aldosterone antagonist, drospirenone may increase the possibility of hyponatremia in high-risk women.
5.15 Exacerbation of Endometriosis
A few cases of malignant transformation of residual endometrial implants have been reported in women treated post-hysterectomy with estrogen-alone therapy.
5.16 Hereditary Angioedema
Exogenous estrogens may exacerbate symptoms of angioedema in women with hereditary angioedema. Consider whether the benefits of estrogen therapy, including Angeliq, outweigh the risks in such women.
5.17 Exacerbation of Other Conditions
Estrogen therapy, including Angeliq, may cause an exacerbation of asthma, diabetes mellitus, epilepsy, migraine, porphyria, systemic lupus erythematosus otosclerosis, chorea minor and hepatic hemangiomas. Consider whether the benefits of estrogen therapy outweigh the risks in women with such conditions.
5.18 Laboratory Tests
Serum follicle stimulating hormone (FSH) and estradiol concentrations have not been shown to be useful in the management of moderate to severe vasomotor symptoms.
5.19 Interference with Laboratory Tests
- •
- Accelerated prothrombin time, partial thromboplastin time, and platelet aggregation time; increased platelet count; increased factors II, VII antigen, VIII antigen, VIII coagulant activity, IX, X, XII, VII–X complex, II–VII–X complex, and beta-thromboglobulin; decreased concentrations of anti-factor Xa and antithrombin III, decreased antithrombin III activity; increased concentrations of fibrinogen and fibrinogen activity; increased plasminogen antigen and activity.
- •
- Increased TBG concentrations leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 concentrations (by column or by radioimmunoassay) or T3 concentrations by radioimmunoassay. T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Women on thyroid replacement therapy may require higher doses of thyroid hormone.
- •
- Other binding proteins may be elevated in serum, for example, corticosteroid binding globulin (CBG), sex hormone binding globulin, leading to increased total circulating corticosteroids and sex steroids, respectively. Free hormone concentrations, such as testosterone and estradiol, may be decreased. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-l-antitrypsin, ceruloplasmin).
- •
- Increased plasma high-density lipoprotein (HDL) and HDL2 subfraction concentrations, reduced low-density lipoprotein (LDL) cholesterol concentration, and increased triglyceride concentrations.
- •
- Impaired glucose tolerance.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed elsewhere in the labeling:
- •
- Cardiovascular Disorders [see Boxed Warning, Warnings and Precautions (5.1)]
- •
- Malignant Neoplasms [see Boxed Warning, Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
From clinical trials with different dose formulations of Angeliq containing E2 dose ranging from 0.5 mg to 1.0 mg combined with DRSP dose ranging from 0.25 mg to 3 mg:
- •
- The most common adverse reactions were gastrointestinal and abdominal pain, female genital bleeding, breast pain and headache. The frequencies of common adverse reactions, in general, were higher for the Angeliq dose formulation containing E2 1 mg compared to Angeliq containing E2 0.5 mg.
- •
- The most common adverse reactions leading to drug discontinuation in controlled clinical trials were abdominal pain, headache, postmenopausal bleeding, breast tenderness, and weight increased.
Placebo-Controlled Trial:
In a placebo-controlled trial evaluating Angeliq 0.25 mg DRSP/0.5 mg E2, 183 postmenopausal women received at least one dose of DRSP 0.25 mg/0.5 mg E2 and 180 received placebo. Study participants were treated for 3 cycles of 28 days each for a total of 12 weeks of treatment. The median age was 53 years (range: 40-77 years) and over 50% of women had a hysterectomy, 68% were Caucasian and 24% were Black. Table 1 summarizes adverse reactions reported in at least 2% of women receiving Angeliq 0.25 mg DRS/0.5 mg E2 and at a higher incidence than subjects receiving placebo.
Table 1: Adverse Reactions that Occurred at a Frequency of ≥ 2% with Angeliq 0.25 mg DRSP/0.5 mg E2 and at a Higher Incidence than Placebo Adverse Reaction
Angeliq
(0.25 mg DRSP/0.5 mg E2)
N=183 (100%)n (%)
Placebo
N=180 (100%)n (%)
Gastrointestinal and abdominal pains*
11 (6.0)
5 (2.8)
Headache
11 (6.0)
9 (5.0)
Vulvovaginal fungal infections
10 (5.5)
1 (0.6)
Breast pain†
6 (3.3)
1 (0.6)
Nausea
6 (3.3)
2 (1.1)
Diarrhea
4 2.2)
1 (0.6)
Peripheral Edema
4 (2.2)
2 (1.1)
Pooled data of clinical trials with different dose formulations of Angeliq:
Data from 13 clinical trials in postmenopausal women treated with different dose formulations of Angeliq containing 1 mg E2 (1 mg E2 + 0.5 mg – 3.0 mg DRSP; N=2842) were pooled to provide an overall estimate of adverse reactions. Similarly, data from 2 clinical trials with Angeliq containing 0.5 mg E2 (0.5 mg E2 + DRSP 0.25 mg – 0.5 mg; N=853) were pooled for the same purpose. Table 2 shows adverse reactions reported in at least 1% of women treated with Angeliq.
Table 2: Adverse Reactions that Occurred at a Frequency of ≥ 1% in Clinical Trials Adverse Reaction
Angeliq containing 1 mg E2
N = 2842
n (%)
Angeliq containing 0.5 mg E2
N=853
n (%)
Breast pain or discomfort
508 (17.9)
53 (6.2)
Female genital tract bleeding
397 (14.0)
21 (2.5)
Gastrointestinal and abdominal pain
186 (6.5)
31 (3.6)
Cervical polyp
34 (1.2)
3 (0.4)
Emotional lability
35 (1.2)
11 (1.3)
Migraine
28 (1.0)
5 (0.6)
Adverse Reactions in clinical studies were coded using the MedDRA dictionary (version 13.0). Different MedDRA terms representing the same medical phenomenon have been grouped together as single adverse reactions to avoid diluting or obscuring the true effect.
6.2 Postmarketing Experience
The following additional adverse reactions have been reported during post-approval use of Angeliq. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establishing a causal relationship to drug exposure.
Immune System Disorders: Hypersensitivity reactions, including rash, pruritis, and urticaria
Reproductive system and breast disorders: Breast cancer
Vascular disorders: venous and arterial thromboembolic events (peripheral deep venous occlusion, thrombosis and embolism/pulmonary vascular occlusion, thrombosis, embolism and infarction/myocardial infarction/cerebral infarction and stroke not specified as hemorrhagic)
-
7 DRUG INTERACTIONS
7.1 Metabolic Interactions
Effect of Drospirenone on Other Drugs
The potential effect of DRSP on CYP2C19 activity was investigated in a clinical pharmacokinetic study using omeprazole as a marker substrate. No significant effect of DRSP on the systemic clearance of the CYP3A4 product omeprazole sulfone was found. These results demonstrated that DRSP did not inhibit CYP2C19 and CYP3A4 in vivo. Two further clinical drug-drug interaction studies using simvastatin and midazolam as marker substrates for CYP3A4, respectively, were performed and the results of these studies demonstrated that pharmacokinetics of the CYP3A4 substrates were not influenced by steady-state DRSP concentrations.
Co-administration of DRSP and drugs that may increase serum potassium: There is a potential for an increase in serum potassium in women taking DRSP with other drugs that may affect electrolytes, such as ACE inhibitors, angiotensin receptor blockers, or NSAIDs, more pronounced in diabetic women [see Warnings and Precautions (5.2), and Clinical Pharmacology (12.3)].
Electrolytes were studied in postmenopausal women with hypertension and/or diabetes mellitus requiring an ACE inhibitor or angiotensin receptor blocker. After 28 days of exposure to 1 mg E2 and 3 mg DRSP (n=112) or placebo (n=118). The mean change from baseline in serum potassium was 0.11 mEq/L for the E2/DRSP group and 0.08 mEq/L for the placebo group. None of the subjects with serum potassium concentrations ≥5.5 mEq/L had cardiovascular adverse events.
A drug-drug interaction study of DRSP 3 mg/E2 1 mg versus placebo was performed in mildly hypertensive postmenopausal women taking enalapril maleate 10 mg twice daily. Potassium concentrations were obtained every other day for a total of 2 weeks in all subjects. Mean serum potassium concentrations in the DRSP/E2 treatment group relative to baseline were 0.22 mEq/L higher than those in the placebo group. On Day 14, the ratios for serum potassium Cmax and AUC in the DRSP/E2 group to those in the placebo group were 0.955 (90% CI: 0.914, 0.999) and 1.01 (90% CI: 0.944, 1.08), respectively. No woman in either treatment group developed hyperkalemia (serum potassium concentrations >5.5 mEq/L).
Of note, occasional or chronic use of NSAID medication was not restricted in any of the Angeliq clinical trials.
Effect of Other Drugs on Estrogens and Progestins
In vitro and in vivo studies have shown that estrogens and progestins are metabolized partially by cytochrome P450 3A4 (CYP3A4). Therefore, inducers or inhibitors of CYP3A4 may affect estrogen drug metabolism. In a clinical drug-drug interaction study conducted in premenopausal women, once daily co-administration of DRSP 3 mg/E2 1.5 mg containing tablets with strong CYP3A4 inhibitor, ketoconazole 200 mg twice daily for 10 days resulted in a moderate increase of exposure and a mild increase of peak concentration for DRSP. The E2 exposure and peak concentration were unaffected by ketoconazole, although the exposure and peak concentration of estrone (E1) increased. Although no clinically relevant effects on any safety or laboratory parameters including serum potassium were observed, this study only assessed women for 10 days. The clinical impact for a woman taking a DRSP-containing combination hormone and chronic use of a CYP3A4/5 inhibitor is unknown.
Substances decreasing the exposure and possibly diminishing the efficacy of estrogens and progestins (enzyme inducers)
Inducers of CYP3A4 such as St. John's wort (Hypericum perforatum), phenobarbital, carbamazepine, and rifampin may reduce plasma concentrations of estrogens and progestins, possibly resulting in a decrease in therapeutic effects and/or changes in the uterine bleeding profile.
Substances increasing the exposure of estrogens and progestins (enzyme inhibitors)
Concomitant administration of moderate or strong CYP3A4 inhibitors such as azole antifungals (for example, ketoconazole, itraconazole, voriconazole, fluconazole), verapamil, macrolides (for example, clarithromycin, erythromycin), diltiazem, and grapefruit juice did increase the plasma concentrations of the estrogen or the progestin or both [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.3)].
HIV/HCV protease inhibitors and non-nucleoside reverse transcriptase inhibitors
Significant changes (increase or decrease) in the plasma concentrations of estrogen and progestin have been noted in some cases of co-administration with HIV/HCV protease inhibitors or with non-nucleoside reverse transcriptase inhibitors.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Angeliq is not indicated for use in pregnancy. There are no data with the use of Angeliq in pregnant women, however, epidemiologic studies and meta-analyses have not found an increased risk of genital or nongenital birth defects (including cardiac anomalies or limb-reduction defects) following exposure to combined hormonal contraceptives (estrogens and progestins) before conception or during early pregnancy.
In reproduction studies in rats, rabbits and monkeys with oral administration of DRSP either as single compound or in combination with EE, no non-genital teratogenicity was observed. Adverse developmental outcomes like an increase in fetal mortality and a retardation of fetal maturation were seen in rats and rabbits at exposures to DRSP exceeding the human exposure by a factor of >15 (in rats) or >60 (rabbits). Related to the antiandrogenic activity of drospirenone, a feminization of male fetuses and an impairment of male fertility was observed in rats (>150 times the human exposure to drospirenone) but not in monkeys (at up to more than 300 times the human exposure to drospirenone). Due to the large safety margins observed in the animal studies only a low likelihood of an increased risk for human pregnancy was concluded (see Data).
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In an embryo-fetal toxicity study in pregnant rats, DRSP was given from day 6 to 15 of gestation orally at doses of 5, 15 and 45 mg/kg/day, more than 60 times the human exposure starting from the low dose based on AUC of DRSP. A slight increase in postimplantational loss and a slight increase in retardation of fetal development (e.g. delayed ossification of bones of the feet) was seen in the two higher doses. No teratogenicity was observed in rats.
In an embryo-fetal study in rabbits, DRSP was given from day 6 to 18 of gestation orally at doses of 10, 30 and 100 mg/kg/day, about 20, 60 and 250 times the human exposure based on AUC. This resulted in a retardation of fetal development (delayed ossification of small bones, multiple fusions of ribs) at the high dose only and in an increase in fetal loss from the mid dose level. No compound-related teratogenicity was seen in rabbits.
In a further embryo-fetal toxicity study in pregnant rats, DRSP was orally administered in combination with ethinyl estradiol (100:1) from day 6 to 17 of gestation at doses of 1, 3 and 10 mg/kg/day DRSP, at about 1, 3 and 23 times the human exposure to DRSP on basis of AUC. Maternal toxicity (decreased body weight gain and food consumption) was seen starting at the low dose and an increase of early resorptions at the high dose level. Skeletal variations and retardations were seen in fetuses at the high dose. No malformed fetuses and no effect on the external genitalia of the fetuses were observed.
DRSP was administered with ethinyl estradiol (100:1) orally to pregnant rats during late pregnancy from day 14 to 21 of gestation (the period of genital development) at doses of 5, 15 and 45 mg/kg of DRSP, more than 60 times the human exposure starting from the low dose based on AUC of DRSP. Maternal toxicity (decreased body weight gain) and fetal retardation (decreased fetal body weights) were seen starting at the low dose. There was a dose dependent increase in feminization of male rat fetuses starting at the mid dose level (that is, >150 times the human exposure to DRSP).
DRSP was administered with ethinyl estradiol (100:1) orally to pregnant cynomolgus monkeys at doses up to 10 mg/kg DRSP, more than 300 times the human exposure based on AUC from day 20 to 90 of gestation. A dose-dependent increase of abortions was observed. No teratogenic or feminization effects were seen in any dose group.
DRSP was administered with ethinyl estradiol (100:1) in a peri-postnatal study in rats from day 6 to 16 of gestation and day 1 to 22 postpartum at doses of 5, 15 and 45 mg/kg; more than 60 times the human exposure starting from the low dose based on AUC of DRSP. There was a dose dependent delay in fetal development and an increase in mortality of the F1-generation during the lactational phase. Fertility was impaired in the male offspring at the high dose level.
8.2 Lactation
Risk Summary
Estrogens plus progestogens are present in human milk and can reduce milk production in breast-feeding women. This reduction can occur at any time but is less likely to occur once breast-feeding is well established. After administration of an oral contraceptive containing DRSP about 0.02% of the DRSP dose was excreted into the breast milk of postpartum women within 24 hours. This results in a maximal daily dose of about 3 mcg DRSP in an infant. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Angeliq and any potential adverse effects on the breastfed infant from Angeliq or from the underlying maternal condition.
8.4 Pediatric Use
Angeliq is not indicated for use in pediatric patients. Clinical studies have not been conducted in the pediatric population.
8.5 Geriatric Use
There have not been sufficient numbers of geriatric women involved in clinical studies utilizing Angeliq to determine whether those over 65 years of age differ from younger women in their response to Angeliq.
The Women’s Health Initiative Studies
In the WHI estrogen plus progestin substudy (daily CE [0.625 mg] plus MPA [2.5 mg] versus placebo), there was a higher relative risk of nonfatal stroke and invasive breast cancer in women greater than 65 years of age [see Warnings and Precautions (5.1, 5.3) and Clinical Studies (14.4)].
In the WHI estrogen-alone substudy (daily CE [0.625 mg] versus placebo), there was a higher relative risk of stroke in women greater than 65 years of age [see Warnings and Precautions (5.1) and Clinical Studies (14.4)].
The Women’s Health Initiative Memory Study
In the WHIMS ancillary studies of postmenopausal women 65 to 79 years of age, there was an increased risk of developing probable dementia in women receiving estrogen plus progestin or estrogen-alone when compared to placebo [see Warnings and Precautions (5.4), and Clinical Studies (14.5)].
Since both ancillary studies were conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women8 [see Warnings and Precautions (5.4), and Clinical Studies (14.5)].
8.6 Renal Impairment
Angeliq is contraindicated in patients with renal impairment because of the risk of hyperkalemia [see Contraindications (4), Warnings and Precautions (5.2) and Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Angeliq tablets, for oral administration, provide a hormone regimen consisting of drospirenone and estradiol.
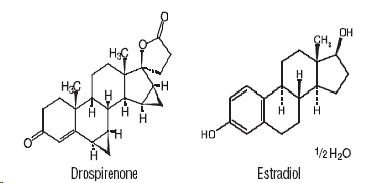
Drospirenone, (6R,7R,8R,9S,10R,13S,14S,15S,16S,17S)-1,3´,4´,6, 6a,7,8,9,10,11,12,13,14,15,15a,16-hexadecahydro-10,13-dimethylspiro-[17H-dicyclopropa[6,7:15,16]cyclopenta[a]phenanthrene- 17,2´(5H)-furan]-3,5´(2H)-dione (CAS) is a synthetic progestational compound and has a molecular weight of 366.5 and a molecular formula of C24H30O3.
Estradiol USP, (Estra-1,3,5(10)-triene-3,17-diol,17ß), has a molecular weight of 272.39 and the molecular formula is C18H24O2. The structural formulas are as follows:
The inactive ingredients in Angeliq 0.5 mg DRSP/1 mg E2 tablets are: lactose monohydrate NF, corn starch NF, pregelatinized starch NF, povidone 25000 USP, magnesium stearate NF, hydroxylpropylmethyl cellulose USP, macrogol 6000 NF, talc USP, titanium dioxide USP, and red ferric oxide pigment NF.
The inactive ingredients in Angeliq 0.25 mg DRSP/0.5 mg E2 tablets are: lactose monohydrate NF, corn starch NF, pregelatinized starch NF, povidone 25000 USP, magnesium stearate NF, hydroxylpropylmethyl cellulose USP, macrogol 6000 NF, talc USP, titanium dioxide USP, and yellow ferric oxide pigment NF.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Endogenous estrogens are largely responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Although circulating estrogens exist in a dynamic equilibrium of metabolic interconversions, estradiol (E2) is the principal intracellular human estrogen and is substantially more potent than its metabolites, estrone and estriol, at the receptor level.
The primary source of estrogen in normally cycling adult women is the ovarian follicle, which secretes 70 to 500 mcg of estradiol daily, depending on the phase of the menstrual cycle. After menopause, most endogenous estrogen is produced by conversion of androstenedione, secreted by the adrenal cortex, to estrone in the peripheral tissues. Thus, estrone and the sulfate-conjugated form, estrone sulfate, are the most abundant circulating estrogens in postmenopausal women.
Estrogens act through binding to nuclear receptors in estrogen-responsive tissues. To date, two estrogen receptors have been identified. These will vary in proportion from tissue to tissue.
Circulating estrogens modulate the pituitary secretion of the gonadotropins, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), through a negative feedback mechanism. Estrogens act to reduce the elevated concentrations of these gonadotropins seen in postmenopausal women.
DRSP is a synthetic progestin and spironolactone analog with antimineralocorticoid activity. In animals and in vitro, drospirenone has antiandrogenic activity, but no glucocorticoid, antiglucocorticoid, estrogenic, or androgenic activity. Progestins counter estrogenic effects by decreasing the number of nuclear estradiol receptors and suppressing epithelial DNA synthesis in endometrial tissue.
12.2 Pharmacodynamics
Generally, a serum estrogen concentration does not predict an individual woman’s therapeutic response to Angeliq nor her risk for adverse outcomes. Likewise, exposure comparisons across different estrogen plus progestin products to infer efficacy or safety for the individual woman may not be valid.
12.3 Pharmacokinetics
Absorption
Serum concentrations of DRSP reach peak concentrations approximately 1 hour after administration of Angeliq and mean absolute bioavailability of DRSP ranges from 76–85%. Following oral administration, the median Tmax of serum estradiol was approximately 2 hours after dosing with Angeliq and Tmax ranged between 0.3-10 hours.
The pharmacokinetics of DRSP are dose proportional within the dose range of 0.25–4 mg. Following daily dosing of Angeliq, steady state DRSP concentrations were observed after 10 days. Mean accumulation ratios for DRSP and estradiol were 2.3 and 2.0, respectively, following multiple doses of 0.5 mg DRSP/1 mg E2, and 2.6 and 1.6, respectively, following multiple doses of 0.25 mg DRSP/0.5 mg E2. Mean concentrations at 2 hours for DRSP ranged between 5.9 and 6.7 ng/mL after treatment with Angeliq (0.5 mg DRSP/1 mg E2) for 365 days. Mean steady state serum DRSP and E2 concentrations are shown in Figure 1, and a summary of primary pharmacokinetic parameters following the administration of 0.25 mg DRSP/0.5 mg E2 or 0.5 mg DRSP/1 mg E2 at steady state is presented in Table 3.
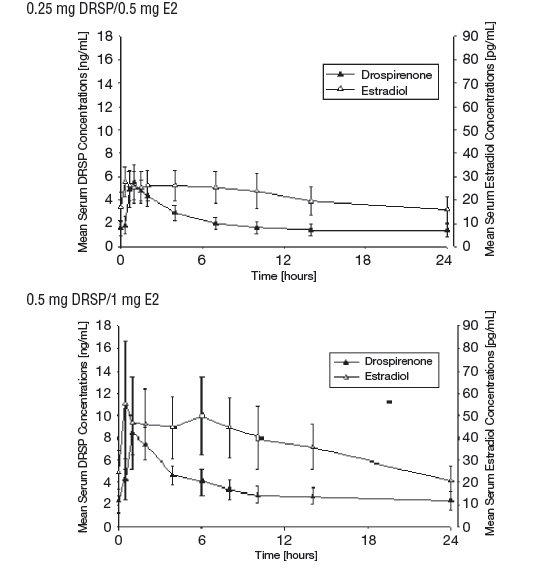
Figure 1: Mean (± SD) steady state serum drospirenone and estradiol concentrations following daily oral administration of 0.25 or 0.5 mg Drospirenone and 0.5 or 1 mg Estradiol
Table 3: Mean (± SD) Steady State Pharmacokinetic Parameters after Administration of Tablets Containing 0.25 or 0.5 mg Drospirenone and 0.5 or 1 mg Estradiol - *
- N=16
Parameter
Unit
0.25 mg DRSP/0.5 mg E2
0.5 mg DRSP/1 mg E2
Drospirenone (DRSP)
N=12
N=17
Cmax
ng/mL
5.70 (1.42)
8.50 (1.63)
Tmax
h
0.992 (0.667 – 1.03)
1.02 (1 – 2.03)
AUC (0-24)
ng·h/mL
48.5 (13.7)
84.3 (19.7)
t1/2
h
N/A
39.2*(8.5)
Estradiol (E2)
Cmax
pg/mL
29.7 (6.80)
63.7 (24.2)
Tmax
h
2.33 (0.32 – 10)
2.01 (0.5 – 6.02)
AUC (0-24)
pg·h/mL
515.4 (142.0)
882 (267)
t1/2
h
N/A
20.5 (2.67)
Estrone (E1)
Cmax
pg/mL
165.7 (40.4)
362 (122)
Tmax
h
3.98 (1.98 – 7.05)
6 (3.99 – 10)
AUC (0-24)
pg·h/mL
2839 (658)
5561 (1689)
t1/2
h
N/A
19.9 (2.10)
Except for Tmax, the mean PK results of DRSP, E2, and E1 are displayed as the arithmetic mean and standard deviation (SD, in parentheses). For Tmax the median and range are provided.
Cmax=Maximum observed serum concentration
Tmax=time to reach Cmax
AUC (0-24)=area under the serum concentration-time curve from 0 h up to 24 h after daily multiple administration
t1/2=half-life
N/A=Not available
Effect of Food
The effect of food on the absorption and bioavailability of DRSP and E2 have not been investigated following the administration of Angeliq. However, clinical studies with different formulations containing DRSP or E2 have shown that the bioavailability of both drugs is not affected by concomitant food intake.
Distribution
The mean volume of distribution of DRSP is 4.2 L/kg. DRSP does not bind to SHBG or CBG but binds about 97% to other serum proteins. The distribution of exogenous estrogens is similar to that of endogenous estrogens. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs. Estradiol circulates in the blood bound to SHBG (37%) and to albumin (61%), while only approximately 1%–2% is unbound.
Metabolism
Mean clearance of DRSP is 1.2 mL/min/kg. DRSP is extensively metabolized after oral administration. The two main metabolites of DRSP found in human plasma were identified to be the acid form of DRSP generated by opening of the lactone ring and the 4,5-dihydrodrospirenone-3-sulfate, formed by reduction and subsequent sulfation. These metabolites were shown not to be pharmacologically active. DRSP is also subject to oxidative metabolism catalyzed by CYP3A4.
Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is a major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women, a significant proportion of the circulating estrogens exist as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.
Excretion
DRSP serum concentrations are characterized by a terminal elimination half-life of approximately 36–42 hours. Excretion of DRSP was nearly complete after 10 days and amounts excreted were slightly higher in feces compared to urine. DRSP was extensively metabolized and only trace amounts of unchanged DRSP were excreted in urine and feces. At least 20 different metabolites were observed in urine and feces. About 38% to 47% of the metabolites in urine were glucuronide and sulfate conjugates. In feces, about 17% to 20% of the metabolites were excreted as glucuronides and sulfates. Estradiol, estrone, and estriol are excreted in the urine along with glucuronide and sulfate conjugates.
Renal Impairment
Angeliq is contraindicated in patients with renal impairment [see Contraindications (4) and Warnings and Precautions (5.2)].
The effect of renal impairment on the pharmacokinetics of DRSP (3 mg daily for 14 days) and the effects of DRSP on serum potassium concentrations were investigated in female subjects (n=28, age 30-65 years) with creatinine clearance (CLcr) ≥ 80 mL/min (11 patients), and CLcr of 50-79 mL/min (10 patients) and CLcr of 30-49 mL/min (7 patients). All subjects were on a low potassium diet. During the study 7 subjects continued the use of potassium-sparing drugs for the treatment of the underlying illness. On the 14th day (steady-state) of DRSP treatment, the serum DRSP concentrations were on average 37% higher in the group with CLcr of 30-49 mL/min compared to those in the group with normal renal function (CLcr ≥ 80 mL/min). Serum DRSP concentrations in the group with CLcr of 50-79 mL/min were comparable to those in the group with CLcr ≥ 80 mL/min. DRSP treatment was well tolerated by all groups. DRSP treatment did not show any clinically significant effect on serum potassium concentration. Although hyperkalemia was not observed in the study, in 5 of the 7 subjects who continued use of potassium sparing drugs during the study, individual mean serum potassium concentrations increased by up to 0.33 mEq/L. Therefore, potential exists for hyperkalemia to occur in subjects with renal impairment whose serum potassium is in the upper reference range, and who are concomitantly using potassium sparing drugs.
Hepatic Impairment
Angeliq is contraindicated in patients with hepatic impairment [see Contraindications (4) and Warnings and Precautions (5.10)]. The mean exposure to DRSP in women with moderate liver impairment is approximately three times the exposure in women with normal liver function.
Effects of Drospirenone on Other Drugs:
Metabolism of DRSP and potential effects of DRSP on hepatic CYP enzymes have been investigated in in vitro and in vivo studies. In in vitro studies, DRSP did not affect turnover of model substrates of CYP1A2 and CYP2D6, but had an inhibitory influence on the turnover of model substrates of CYP1A1, CYP2C9, CYP2C19 and CYP3A4 with CYP2C19 being the most sensitive enzyme.
The potential effect of DRSP on CYP2C19 activity was investigated in a clinical pharmacokinetic study using omeprazole as a marker substrate. In the study with 24 postmenopausal women [including 12 women with homozygous (wild type) CYP2C19 genotype and 12 women with heterozygous CYP2C19 genotype] the daily oral administration of 3 mg DRSP for 14 days did not affect the systemic clearance of the CYP2C19 substrate omeprazole (40 mg) and the CYP2C19 product 5-hydroxy-omeprazole. Furthermore, no significant effect of DRSP on the systemic clearance of the CYP3A4 product omeprazole sulfone was found. These results demonstrated that DRSP did not inhibit CYP2C19 and CYP3A4 in vivo.
Two further clinical drug-drug interaction studies using simvastatin and midazolam as marker substrates for CYP3A4 were each performed in 24 healthy, postmenopausal women. The results of these studies demonstrated that pharmacokinetics of the CYP3A4 substrates were not influenced by steady-state DRSP concentrations achieved after administration of 3 mg DRSP/day.
Based on the available results of in vivo and in vitro studies, it can be concluded that, at clinical dose concentration, DRSP is unlikely to inhibit significantly CYP enzymes.
There is a potential for an increase in serum potassium in women taking drospirenone with other drugs that may affect electrolytes, such as ACE inhibitors, angiotensin receptor blockers, or NSAIDs.
Electrolytes were studied in 230 postmenopausal women with hypertension and/or diabetes mellitus requiring an ACE inhibitor or angiotensin receptor blocker. Of these, 26 patients had a creatinine clearance >50 mL/min to <80 mL/min. Patients were given 1 mg E2 and 3 mg DRSP (n=112) or placebo (n=118) over 28 days. Non-diabetic patients also received ibuprofen 1200 mg/day for 5 days during the study. There was a single case of serum potassium >6 mEq/L and a single case of serum sodium <130 mEq/L on treatment, both occurring following five days of ibuprofen therapy in two women taking E2/DRSP. Serum potassium concentrations ≥5.5 mEq/L were observed in 8 (7.3%) E2/DRSP-treated women (3 diabetic and 5 non-diabetic) and in 3 (2.6%) placebo-treated subjects (2 diabetic and 1 non-diabetic). After 28 days of exposure, the mean change from baseline in serum potassium was 0.11 mEq/L for the E2/DRSP group and 0.08 mEq/L for the placebo group. None of the subjects with serum potassium concentrations ≥5.5 mEq/L had cardiovascular adverse events.
A drug-drug interaction study of DRSP 3 mg/E2 1 mg versus placebo was performed in 24 mildly hypertensive postmenopausal women taking enalapril maleate 10 mg twice daily. Potassium concentrations were obtained every other day for a total of 2 weeks in all subjects. Mean serum potassium concentrations in the DRSP/E2 treatment group relative to baseline were 0.22 mEq/L higher than those in the placebo group. Serum potassium concentrations also were measured at multiple timepoints over 24 hours at baseline and on Day 14. On Day 14, the ratios for serum potassium Cmax and AUC in the DRSP/E2 group to those in the placebo group were 0.955 (90% CI: 0.914, 0.999) and 1.01 (90% CI: 0.944, 1.08), respectively. No patient in either treatment group developed hyperkalemia (serum potassium concentrations >5.5 mEq/L).
Of note, occasional or chronic use of NSAID medication was not restricted in any of the Angeliq clinical trials.
Effects of Other Drugs on Estrogens and Progestins:
In vitro and in vivo studies have shown that estrogens and progestins are metabolized partially by CYP3A4. Therefore, inducers or inhibitors of CYP3A4 may affect estrogen and progestin drug metabolism [see Drug Interactions (7.1)]. In a clinical drug-drug interaction study conducted in 18 premenopausal women, once daily co-administration of DRSP 3 mg/E2 1.5 mg combination tablets with strong CYP3A4 inhibitor, ketoconazole 200 mg twice daily for 10 days resulted in a 2.30-fold (90% CI: 2.08-2.54) increase of the AUC (0-24) and a 1.66-fold (90% CI: 1.50-1.84) increase of Cmax for DRSP. The E2 exposure [that is, AUC (0-24) and Cmax] was unaffected by ketoconazole, although the AUC(0-24) and Cmax for E1 increased 1.39-fold (90% CI: 1.27-1.52) and 1.32-fold (90% CI: 1.23-1.42), respectively.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 24-month oral carcinogenicity study in mice dosed with 10 mg/kg/day DRSP alone or 1+0.01, 3+0.03 and 10+0.1 mg/kg/day of DRSP and ethinyl estradiol, 0.24 to 10.3 times the exposure (AUC of drospirenone) of women taking a 1 mg dose, there was an increase in carcinomas of the Harderian gland in the group that received the high dose of drospirenone alone. In a similar study in rats given 10 mg/kg/day drospirenone alone or 0.3+0.003, 3+0.03 and 10+0.1 mg/kg/day drospirenone and ethinyl estradiol, 2.3 to 51.2 times the exposure of women taking a 1 mg dose, there was an increased incidence of benign and total (benign and malignant) adrenal gland pheochromocytomas in the group receiving the high dose of drospirenone. Drospirenone was not mutagenic in a number of in vitro (Ames, Chinese Hamster Lung gene mutation and chromosomal damage in human lymphocytes) and in vivo (mouse micronucleus) genotoxicity tests. Drospirenone increased unscheduled DNA synthesis in rat hepatocytes and formed adducts with rodent liver DNA but not with human liver DNA.
-
14 CLINICAL STUDIES
14.1 Effects on Vasomotor Symptoms in Postmenopausal Women
Angeliq 0.25 mg DRSP/0.5 mg E2
The efficacy of Angeliq 0.25 mg DRSP/0.5 mg E2 for reducing the frequency and severity of moderate to severe vasomotor symptoms was evaluated in a randomized, double-blind, placebo-controlled trial. A total of 735 postmenopausal women ≥ 40 years of age with a minimum of 7 to 8 moderate to severe hot flashes daily or 50 to 60 moderate to severe hot flashes weekly were randomized to one of the two doses of Angeliq, including DRSP 0.25 mg/0.5 mg E2, estrogen monotherapy, or placebo. The median age of study participants was 53 years and 68% were Caucasian. Efficacy for vasomotor symptoms was assessed during the 12 weeks of treatment. Compared to placebo, women receiving Angeliq 0.25 mg DRSP/0.5 mg E2 achieved statistically significant reduction in the frequency and severity of moderate to severe vasomotor symptoms at Week 4 and at Week 12. The mean difference in daily reduction of frequency of hot flushes between Angeliq 0.25 mg DRSP/0.5 mg E2 and placebo were approximately -2 episodes at Week 4 and -3 episodes at Week 12. Table 4 shows the mean number of hot flushes in the Angeliq 0.25 mg DRSP/0.5 mg E2 and placebo groups and the treatment difference between Angeliq 0.25 mg DRSP/0.5 mg E2 and placebo treatment at Week 4 and at Week 12.
Table 4: Summary Tabulation of the Number of Hot Flushes Per Day - Mean Values and Comparisons Between the Active Treatment Group and the Placebo Group, Last Observation Carried Forward - *
- Mean change from baseline, difference from placebo, 95% confidence interval, and p-value based on an ANCOVA model with treatment and pooled center as factors and baseline measurement as covariate
Treatment
No. of Hot Flushes/Day
Time Period
(week)Baseline
MeanMean Change from Baseline*
Difference from Placebo (95% CI)
p-Values
vs. Placebo*DRSP/E2 (0.25 mg/0.5 mg) [n=175]
Week 4
10.68
-5.46
-2.02 (-2.89, -1.16)
<0.0001
Week 12
10.68
-7.71
-3.17 (-3.97, -2.37)
<0.0001
Placebo [n=176]
Week 4
10.53
-3.44
-
-
Week 12
10.53
-4.54
-
-
Angeliq 0.5 mg DRSP/1 mg E2
Support for treatment of vasomotor symptoms and vaginal and vulvar atrophy was shown through bioequivalence of the E2 component of the Angeliq combination product with a currently marketed 1 mg E2 product. The multiple-dose bioequivalence study evaluated the bioequivalence of E2 from a tablet containing DRSP (2 mg) and E2 (1 mg) relative to E2 1 mg tablet. Angeliq 0.5 mg DRSP/1 mg E2 tablets met the criteria for bioequivalence to the E2 1 mg comparator.
14.2 Effects on Endometrium in Postmenopausal Women
Angeliq 0.25 mg DRSP/0.5 mg E2
In a one year clinical trial, 661 postmenopausal women were treated with Angeliq 0.25 mg DRSP/0.5 mg E2 (N=489) or a comparator drug (N=172). Endometrial biopsies were performed on 407 (83.2%) women in the Angeliq group during the treatment period. No endometrial hyperplasias occurred during or after one year of treatment. See Table 5.
Angeliq 0.5 mg DRSP/1 mg E2
In a one year clinical trial of 1,142 postmenopausal women treated with 1 mg E2 alone or 1 mg E2 + 0.5, 1, 2, or 3 mg DRSP, endometrial biopsies were performed on 966 (84.6%) women during the treatment period. Eight women in the E2 monotherapy group developed endometrial hyperplasia (4 simple hyperplasia with no cytological atypia, 3 complex hyperplasia with no cytological atypia, and 1 complex hyperplasia with cytological atypia), and one woman in the 1 mg E2+2 mg DRSP group developed simple hyperplasia with no cytological atypia. Table 5 shows that there were no diagnoses of endometrial hyperplasia in the Angeliq group.
Table 5: Incidence of Endometrial Hyperplasia after up to 12 Months of Treatment - *
- Includes evaluable and unevaluable endometrial biopsy results
E2 1 mg
Angeliq 0.25 mg DRSP/
0.5 mg E2Angeliq 0.5 mg DRSP/
1 mg E2Total No. Subjects Treated
226
489
227
Total No. of
On-Treatment Biopsies*197 (87.2%)
407 (83.2%)
191 (84.1%)
Hyperplasia
8 (4%)
0 (0%)
0 (0%)
14.3 Effects on Uterine Bleeding or Spotting in Postmenopausal Women
Angeliq 0.5 mg DRSP/1 mg E2 and Angeliq 0.25 mg DRSP /0.5 mg E2 were evaluated in separate one-year clinical trials investigating the endometrial safety in postmenopausal women with an intact uterus.
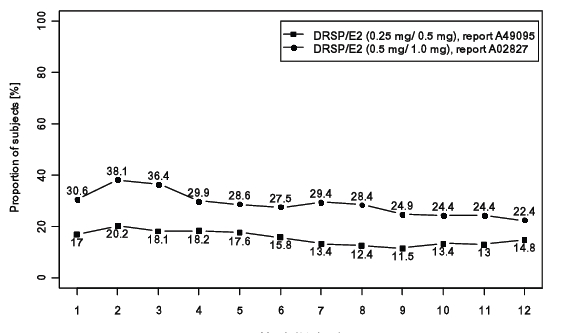
Over 12 months in the double-blind trials, the proportions of women with any bleeding or spotting decreased over time. At one year, approximately 22% of women treated with Angeliq 0.5 mg/E2 1.0 mg and 15% of women treated with Angeliq 0.25 mg/E2 0.5 mg had any uterine bleeding or spotting. See Figure 2.
14.4 Women's Health Initiative Studies
The WHI enrolled approximately 27,000 predominantly healthy postmenopausal women in two substudies to assess the risks and benefits of daily oral CE (0.625 mg)-alone or in combination with MPA (2.5 mg) compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of CHD defined as nonfatal MI, silent MI and CHD death], with invasive breast cancer as the primary adverse outcome. A "global index" included the earliest occurrence of CHD, invasive breast cancer, stroke, PE, endometrial cancer (only in the CE plus MPA substudy), colorectal cancer, hip fracture, or death due to other cause. These substudies did not evaluate the effects of CE plus MPA or CE-alone on menopausal symptoms.
WHI Estrogen plus Progestin Substudy
The WHI estrogen plus progestin substudy was stopped early. According to the predefined stopping rule, after an average follow-up of 5.6 years of treatment, the increased risk of breast cancer and cardiovascular events exceeded the specified benefits included in the "global index." The absolute excess risk of events included in the “global index” was 19 per 10,000 women-years.
For those outcomes included in the WHI “global index” that reached statistical significance after 5.6 years of follow-up, the absolute excess risks per 10,000 women-years in the group treated with CE plus MPA were 7 more CHD events, 8 more strokes, 10 more PEs, and 8 more invasive breast cancers, while the absolute risk reductions per 10,000 women-years were 6 fewer colorectal cancers and 5 fewer hip fractures.
Results of the CE plus MPA substudy, which included 16,608 women (average 63 years of age, range 50 to 79; 83.9 percent White, 6.8 percent Black, 5.4 percent Hispanic, 3.9 percent Other) are presented in Table 6. These results reflect centrally adjudicated data after an average follow-up of 5.6 years.
Table 6: Relative and Absolute Risk Seen in the Estrogen Plus Progestin Substudy of WHI at an Average of 5.6 Years*† - *
- Adapted from numerous WHI publications. WHI publications can be viewed at www.nhlbi.nih.gov/whi.
- †
- Results are based on centrally adjudicated data.
- ‡
- Nominal confidence intervals unadjusted for multiple looks and multiple comparisons.
- §
- Not included in "global index.”
- ¶
- Includes metastatic and non-metastatic breast cancer, with the exception of in situ breast cancer.
- #
- All deaths, except from breast or colorectal cancer, definite or probable CHD, PE or cerebrovascular disease.
- Þ
- A subset of the events was combined in a "global index", defined as the earliest occurrence of CHD events, invasive breast cancer, stroke, pulmonary embolism, colorectal cancer, hip fracture, or death due to other causes.
Event
Relative Risk
CE/MPA vs. Placebo
(95% nCI‡)
CE/MPA
n=8,506
Placebo
n=8,102
Absolute Risk per 10,000 Women-Years
CHD events
1.23 (0.99–1.53)
41
34
Non-fatal MI
1.28 (1.02–1.632)
31
25
CHD death
1.10 (0.70–1.75)
8
8
All strokes
1.31 (1.03–1.68)
33
25
Ischemic stroke
1.44 (1.09-1.90)
26
18
Deep vein thrombosis§
1.95 (1.43-2.67)
26
13
Pulmonary embolism
2.13 (1.45–3.11)
18
8
Invasive breast cancer¶
1.24 (1.01-1.54)
41
33
Colorectal cancer
0.61 (0.42–0.87)
10
16
Endometrial cancer§
0.81 (0.48–1.36)
6
7
Cervical cancer§
1.44 (0.47-4.42)
2
1
Hip fracture‡
0.67 (0.47–0.96)
11
16
Vertebral fractures§
0.65 (0.46–0.92)
11
17
Lower arm/wrist fractures§
0.71 (0.59-0.85)
44
62
Total fractures§
0.76 (0.69-0.83)
152
199
Overall Mortality#
1.00 (0.83-1.19)
52
52
Global IndexÞ
1.13 (1.02-1.25)
184
165
Timing of the initiation of estrogen therapy relative to the start of menopause may affect the overall risk benefit profile. The WHI estrogen plus progestin substudy stratified by age showed in women 50-59 years of age, a non-significant trend toward reduced risk for overall mortality [HR 0.69 (95 percent CT 0.44-1.07)].
WHI Estrogen-Alone Substudy
The WHI estrogen-alone substudy was stopped early because an increased risk of stroke was observed, and it was deemed that no further information would be obtained regarding the risks and benefits of estrogen alone in predetermined primary endpoints.
Results of the estrogen-alone substudy, which included 10,739 women (average age of 63 years, range 50 to 79; 75.3 percent White, 15.1 percent Black, 6.1 percent Hispanic, 3.6 percent Other), after an average follow-up of 7.1 years are presented in Table 7.
Table 7. Relative and Absolute Risk Seen in the Estrogen-Alone Substudy of WHI* - *
- Adapted from numerous WHI publications. WHI publications can be viewed at www.nhlbi.nih.gov/whi.
- †
- Nominal confidence intervals unadjusted for multiple looks and multiple comparisons.
- ‡
- Results are based on centrally adjudicated data for an average follow-up of 7.1 years.
- §
- Not included in “global index.”
- ¶
- Results are based on an average follow-up of 6.8 years.
- #
- All deaths, except from breast or colorectal cancer, definite or probable CHD, PE or cerebrovascular disease.
- Þ
- A subset of the events was combined in a "global index," defined as the earliest occurrence of CHD events, invasive breast cancer, stroke, pulmonary embolism, colorectal cancer, hip fracture, or death due to other causes.
Event
Relative Risk
CE vs. Placebo
(95% nCI†)CE
n=5,310Placebo
n=5,429Absolute Risk per 10,000 Women-Years
CHD events‡
0.95 (0.78–1.16)
54
57
Non-fatal MI‡
0.91 (0.73–1.14)
40
43
CHD death‡
1.01 (0.71–1.43)
16
16
All stroke‡
1.33 (1.05–1.68)
45
33
Ischemic‡
1.55 (1.19-2.01)
38
25
1.47 (1.06-2.06)
23
15
Pulmonary embolism‡
1.37 (0.90–2.07)
14
10
Invasive breast cancer‡
0.80 (0.62-1.04)
28
34
Colorectal cancer‡
1.08 (0.75–1.55)
17
16
Hip fracture‡
0.65 (0.45–0.94)
12
19
0.64 (0.44–0.93)
11
18
0.58 (0.47-0.72)
35
59
0.71 (0.64–0.8)
144
197
1.08 (0.88-1.32)
53
50
1.04 (0.88-1.22)
79
75
Global IndexÞ
1.02 (0.92-1.13)
206
201
For those outcomes included in the WHI "global index" that reached statistical significance, the absolute excess risk per 10,000 women-years in the group treated with CE-alone was 12 more strokes, while the absolute risk reduction per 10,000 women-years was 7 fewer hip fractures.9 The absolute excess risk of events included in the "global index" was a non-significant 5 events per 10,000 women-years. There was no difference between the groups in terms of all-cause mortality.
No overall difference for primary CHD events (nonfatal MI, silent MI and CHD death) and invasive breast cancer incidence in women receiving CE-alone compared with placebo was reported in final centrally adjudicated results from the estrogen-alone substudy, after an average follow-up of 7.1 years.
Centrally adjudicated results for stroke events from the estrogen-alone substudy, after an average follow-up of 7.1 years, reported no significant difference in distribution of stroke subtype or severity, including fatal strokes, in women receiving CE-alone compared to placebo. Estrogen-alone increased the risk for ischemic stroke, and this excess risk was present in all subgroups of women examined.10
Timing of the initiation of estrogen therapy relative to the start of menopause may affect the overall risk benefit profile. The WHI estrogen-alone substudy stratified by age showed in women 50 to 59 years of age, a non-significant trend toward reduced risk for CHD [HR 0.63 (95 percent CI 0.36-1.09)] and overall mortality [HR 0.71 (95 percent CT 0.46-1.11)].
14.5 Women's Health Initiative Memory Study
The WHIMS estrogen plus progestin ancillary study of WHI enrolled 4,532 predominantly healthy postmenopausal women 65 years of age and older (47 percent were 65 to 69 years of age, 35 percent were 70 to 74 years of age, and 18 percent were 75 years of age and older) to evaluate the effects of daily CE (0.625 mg) plus MPA (2.5 mg) on the incidence of probable dementia (primary outcome) compared to placebo.
After an average follow-up of 4 years, the relative risk of probable dementia for CE plus MPA versus placebo was 2.05 (95 percent CI 1.21-3.48). The absolute risk of probable dementia for CE plus MPA was 45 versus 22 cases per 10,000 women-years. Probable dementia as defined in this study included Alzheimer’s disease (AD, vascular dementia (VaD) and mixed type (having features of both AD and VaD). The most common classification of probable dementia in the treatment group and the placebo group was AD. Since the ancillary study was conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.4), and Use in Specific Populations (8.5)].
The WHIMS estrogen-alone ancillary study of WHI enrolled 2,947 predominantly healthy hysterectomized postmenopausal women 65 to 79 years of age and older (45 percent were age 65 to 69 years of age, 36 percent were 70 to 74 years of age, and 19 percent were 75 years of age and older) to evaluate the effects of daily CE (0.625 mg) on the incidence of probable dementia (primary outcome) compared to placebo.
After an average follow-up of 5.2 years, the relative risk of probable dementia for CE-alone versus placebo was 1.49 (95 percent CI, 0.83 - 2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years. Probable dementia as defined in this study included AD, VaD, and mixed type (having features of both AD and VaD). The most common classification of probable dementia in the treatment group and placebo group was AD. Since the ancillary study was conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.4) and Use in Specific Populations (8.5)].
When data from the two populations were pooled as planned in the WHIMS protocol, the reported overall RR for probable dementia was 1.76 (95 percent CI 1.19-2.60). Differences between groups became apparent in the first year of treatment. It is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.4) and Use in Specific Populations (8.5)].
-
15 REFERENCES
- 1.
- Rossouw JE, et al. Postmenopausal Hormone Therapy and Risk of Cardiovascular Disease by Age and Years Since Menopause. JAMA. 2007;297:1465-1477.
- 2.
- Hsia J, et al. Conjugated Equine Estrogens and Coronary Heart Disease. Arch Int Med. 2006;166:357-365.
- 3.
- Cushman M, et al. Estrogen Plus Progestin and Risk of Venous Thrombosis. JAMA. 2004;292:1573-1580
- 4.
- Curb JD, et al. Venous Thrombosis and Conjugated Equine Estrogen in Women Without a Uterus. Arch Int Med. 2006;166:772-780.
- 5.
- Chlebowski RT, et al. Influence of Estrogen Plus Progestin on Breast Cancer and Mammography in Healthy Postmenopausal Women. JAMA. 2003;289:3234-3253.
- 6.
- Stefanick ML, et al. Effects of Conjugated Equine Estrogens on Breast Cancer and Mammography Screening in Postmenopausal Women With Hysterectomy. JAMA. 2006;295:1647-1657.
- 7.
- Anderson GL, et al. Effects of Estrogen Plus Progestin on Gynecologic Cancers and Associated Diagnostic Procedures. JAMA. 2003;290:1739-1748.
- 8.
- Shumaker SA, et al. Conjugated Equine Estrogens and Incidence of Probable Dementia and Mild Cognitive Impairment in Postmenopausal Women. JAMA. 2004;291:2947-2958.
- 9.
- Jackson RD, et al. Effects of Conjugated Equine Estrogen on Risk of Fractures and BMD in Postmenopausal Women With Hysterectomy: Results From the Women's Health Initiative Randomized Trial. J Bone Miner Res. 2006;21:817-828.
- 10.
- Hendrix SL, et al. Effects of Conjugated Equine Estrogen on Stroke in the Women's Health Initiative. Circulation. 2006;113:2425-2434.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Advise patients to read the FDA-Approved patient labeling (Patient Information).
Abnormal Vaginal Bleeding
Inform postmenopausal women to report any vaginal bleeding to their healthcare provider as soon as possible [see Warning and Precautions (5.3)].
Possible Serious Adverse Reactions with Estrogen Plus Progestogen Therapy
Inform postmenopausal women of possible serious adverse reactions of estrogen plus progestogen therapy including cardiovascular disorders, malignant neoplasms, and probable dementia [see Warning and Precautions (5.1, 5.3, 5.4)].
Possible Common Adverse Reactions with Estrogen Plus Progestogen Therapy
Inform postmenopausal women of possible less serious but common adverse reactions of estrogen plus progestogen therapy such as headache, breast pain and tenderness, nausea and vomiting [see Adverse Reactions (6)].
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
Angeliq®(an"ju–le–k')
(drospirenone and estradiol)Tablets
Read this Patient Information before you start using Angeliq and read what you get each time you get a refill your Angeliq prescription. There may be new information. This information does not take the place of talking to your healthcare provider about your menopausal symptoms or your treatment.
What is the most important information I should know about Angeliq
(a combination of estrogen and progestogen)?- •
- Do not use estrogens with or without progestogens to prevent heart disease, heart attacks, strokes, or dementia (declines of brain function).
- •
- Using estrogens with progestogens may increase your chances of getting heart attacks, strokes, breast cancer, or blood clots.
- •
- Using estrogens with progestogen may increase your chance of getting dementia, based on a study of women 65 years of age and older
- •
- Using estrogen-alone may increase your chance of getting cancer of the uterus (womb).
- •
- Do not use estrogen-alone to prevent heart disease, heart attacks, strokes, or dementia (decline in brain function).
- •
- Using estrogen-alone may increase your chances of getting strokes or blood clots
- •
- Using estrogen-alone may increase your chance of getting dementia, based on a study of women 65 years of age and older
- •
- Only one estrogen with progestogen product and dose have been shown to increase your chances of getting heart attacks, strokes, breast cancer, and dementia. Only one estrogen-alone product and dose have been shown to increase your chances of getting strokes, blood clots, and dementia.
- Because other products and doses have not been studied in the same way, it is not known how the use of Angeliq will affect your chances of these conditions. You and your healthcare provider should talk regularly about whether you still need treatment with Angeliq.
What is Angeliq?
Angeliq is a prescription medicine that contains two kinds of hormones, an estrogen and a progestogen.
- •
- Angeliq 0.25 mg drospirenone (DRSP)/0.5 mg estradiol (E2) and Angeliq 0.5 mg DRSP/1 mg E2 are both used after menopause to reduce moderate to severe hot flashes.
- Estrogens are hormones made by a woman's ovaries. The ovaries normally stop making estrogens when a woman is between 45 to 55 years old. This drop in body estrogen levels causes the "change of life" or menopause (the end of monthly menstrual periods). Sometimes, both ovaries are removed during an operation before natural menopause takes place. The sudden drop in estrogen levels causes "surgical menopause."
- When the estrogen levels begin dropping, some women develop very uncomfortable symptoms, such as feelings of warmth in the face, neck, and chest, or sudden intense feelings of heat and sweating ("hot flashes" or "hot flushes"). In some women, the symptoms are mild, and they will not need to use estrogens. In other women, symptoms can be more severe. You and your healthcare provider should talk regularly about whether you still need treatment with Angeliq.
- •
- Angeliq 0.5 mg drospirenone (DRSP)/1 mg estradiol (E2) is used after menopause to treat menopausal changes in or around the vagina. You and your healthcare provider should talk regularly about whether you still need treatment with Angeliq to control these problems. If you use Angeliq only to treat your menopausal changes in and around your vagina, talk with your healthcare provider about whether a topical vaginal product would be better for you.
Who should not use Angeliq?
Do not start using Angeliq if you:
- •
- have had your uterus (womb) removed (hysterectomy). Angeliq contains a progestogen to decrease the chances of getting cancer of the uterus. If you do not have a uterus, you do not need a progestogen and you should not use Angeliq.
- •
- have unusual vaginal bleeding. Vaginal bleeding after menopause may be a warning sign of cancer of the uterus (womb). Your healthcare provider should check any unusual vaginal bleeding to find out the cause.
- •
- Have been diagnosed with a bleeding disorder.
- •
- currently have or have had certain cancers. Estrogens may increase the chances of getting certain types of cancers, including cancer of the breast or uterus. If you have or had cancer, talk with your healthcare provider about whether you should use Angeliq.
- •
- currently have or have had blood clots.
- •
- Had a stroke or heart attack
- •
- have kidney disease, liver disease, or disease of your adrenal glands. Angeliq contains drospirenone which may increase the potassium level in your blood. Liver, kidney, or adrenal gland disease may also increase the potassium level in your blood.
- •
- are allergic to Angeliq or any of its ingredients. See the list of ingredients in Angeliq at the end of this leaflet.
Before you use Angeliq, tell your healthcare provider if you:
- •
- have or have had problems with your adrenal glands
- •
- have high levels of fat in your blood (triglycerides)
- •
-
have any other medical conditions that may become worse while you are using Angeliq Your healthcare provider may need to check you more carefully if you have certain conditions, such as:
- o
- asthma (wheezing)
- o
- epilepsy (seizures)
- o
- diabetes
- o
- migraine
- o
- endometriosis
- o
- lupus
- o
- hypertension (high blood pressure)
- o
- problems with your heart, liver, thyroid or kidneys
- o
- benign breast disease
- o
- have high calcium in your blood
- o
- have high potassium levels in your blood
- o
- have low sodium levels in your blood
- •
- •
- are pregnant or think you may be pregnant
- Angeliq is not for pregnant women.
- •
- are going to have surgery or will be on bed rest. Your healthcare provider will let you know if you need to stop using Angeliq.
- •
- are breastfeeding
- The hormones in Angeliq can pass into your milk.
- Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some medicines may affect how Angeliq works. Some other medicines and food products may increase or decrease the concentrations of the hormones in Angeliq in the blood. Angeliq may also affect how your other medicines work. Angeliq may increase the potassium level in your blood and some medicines may also increase potassium level. In some situations, your healthcare provider may recommend testing your blood for potassium level.
- Keep a list of your medicines and show it to your doctor and pharmacist when you get a new medicine.
How should I use Angeliq?
- •
- Take one Angeliq tablet at the same time each day.
- •
- Take Angeliq tablets whole. Do not break, crush, dissolve, or chew Angeliq tablets before swallowing. If you cannot swallow Angeliq tablets whole, tell your healthcare provider. You may need a different medicine.
- •
- If you miss a dose of Angeliq, take it as soon as possible.
- •
- If more than 24 hours have passed since you missed a dose of Angeliq, you should not take the missed dose.
- •
- Estrogens should be used at the lowest dose possible for your treatment only as long as needed. You and your healthcare provider should talk regularly (for example, every 3 to 6 months) about whether you still need treatment with Angeliq.
What are the possible side effects of Angeliq?
Side effects are grouped by how serious they are and how often they happen when you are treated.
Serious but less common side effects include:
- •
- Heart attack
- •
- Stroke
- •
- Blood clots
- •
- High potassium levels in your blood (hyperkalemia)
- •
- Cancer of the lining of the uterus (womb)
- •
- Breast cancer
- •
- Cancer of the ovary
- •
- Dementia
- •
- Gallbladder disease
- •
- High or low blood calcium
- •
- High blood pressure
- •
- High levels of fat (triglycerides) in your blood
- •
- Liver problems
- •
- Changes in your thyroid hormone levels
- •
- Fluid retention
- •
- Enlargement of benign tumors of the uterus (“fibroids”)
- •
- Worsening of swelling of face and tongue (angioedema) in women with a history of angioedema
Call your healthcare provider right away if you have any of the following warning signs or any other unusual symptoms that concern you:
- •
- New breast lumps
- •
- Changes in vision or speech
- •
- Unusual vaginal bleeding
- •
- Sudden new severe headaches
- •
- Severe pains in your chest or legs with or without shortness of breath, weakness and fatigue
Common side effects of Angeliq include:
- •
- Headache
- •
- Breast pain
- •
- Irregular vaginal bleeding or spotting
- •
- Stomach or abdominal pain
- •
- Nausea
- •
- Diarrhea
- •
- Vaginal yeast infection
- •
- Fluid Retention
- •
- Moodiness
These are not all the possible side effects of Angeliq. For more information, ask your healthcare provider or pharmacist about side effects.
You may report side effects to Bayer HealthCare Pharmaceuticals at 1-888-842-2937 or to FDA at
1-800-FDA-1088.How should I store Angeliq?
Store Angeliq at room temperature between 68˚F to 77˚F (20˚C to 25˚C).
Keep Angeliq and all medicines out of the reach of children.
What can I do to lower my chances of a serious side effect with Angeliq?
- •
- Talk with your healthcare provider regularly about whether you should continue using Angeliq.
- •
- If you have a uterus, talk with your healthcare provider about whether Angeliq is right for you.
- •
- In general, the addition of a progestogen is recommended for a women with a uterus to reduce the chances of getting cancer of the uterus (womb).
- •
- See your healthcare provider right away if you get vaginal bleeding while using Angeliq.
- •
- Have a pelvic exam, breast exam and mammogram (breast X-ray) every year unless your healthcare provider tells you something else. If members of your family have had breast cancer or if you have ever had breast lumps or an abnormal mammogram, you may need to have breast exams more often.
- •
- If you have high blood pressure, high cholesterol (fat in the blood), diabetes, are overweight, or if you use tobacco, you may have higher chances for getting heart disease. Ask your healthcare provider for ways to lower your chances for getting heart disease.
General information about the safe and effective use of Angeliq.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Angeliq for conditions for which it was not prescribed. Do not give Angeliq to other people, even if they have the same symptoms you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about Angeliq that is written for health professionals.
For more information, go to www.angeliq-us.com by or calling our toll free number (1-888-842-2937).
What are the ingredients in Angeliq?
Active ingredients: drospirenone (a progestin) and estradiol.
Inactive ingredients 0.5 mg DRSP/1 mg E2 tablets: lactose monohydrate NF, corn starch NF, pregelatinized starch NF, povidone 25000 USP, magnesium stearate NF, hydroxylpropylmethyl cellulose USP, macrogol 6000 NF, talc USP, titanium dioxide USP, and ferric oxide pigment NF.
Inactive ingredients in 0.25 mg DRSP/0.5 mg E2 tablets: lactose monohydrate NF, corn starch NF, pregelatinized starch NF, povidone 25000 USP, magnesium stearate NF, hydroxylpropylmethyl cellulose USP, macrogol 6000 NF, talc USP, titanium dioxide USP, and yellow ferric oxide pigment NF.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Bayer HealthCare Pharmaceuticals Inc.
Whippany, NJ 07981©2015 Bayer HealthCare Pharmaceuticals Inc
All rights reserved.
October 2023
- PRINCIPAL DISPLAY PANEL
- Angeliq 0.25 mg Trade Carton
-
INGREDIENTS AND APPEARANCE
ANGELIQ
drospirenone and estradiol tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:50419-483 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ESTRADIOL (UNII: 4TI98Z838E) (ESTRADIOL - UNII:4TI98Z838E) ESTRADIOL 1 mg DROSPIRENONE (UNII: N295J34A25) (DROSPIRENONE - UNII:N295J34A25) DROSPIRENONE 0.5 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) FERRIC OXIDE RED (UNII: 1K09F3G675) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) MAGNESIUM STEARATE (UNII: 70097M6I30) POVIDONE K25 (UNII: K0KQV10C35) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color PINK Score no score Shape ROUND (biconvex) Size 6mm Flavor Imprint Code CK Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:50419-483-03 3 in 1 CARTON 02/29/2012 1 NDC:50419-483-01 28 in 1 BLISTER PACK; Type 0: Not a Combination Product 2 NDC:50419-483-72 1 in 1 CARTON 02/29/2012 2 NDC:50419-483-71 14 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021355 11/28/2005 ANGELIQ
drospirenone and estradiol tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:50419-482 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ESTRADIOL (UNII: 4TI98Z838E) (ESTRADIOL - UNII:4TI98Z838E) ESTRADIOL 0.5 mg DROSPIRENONE (UNII: N295J34A25) (DROSPIRENONE - UNII:N295J34A25) DROSPIRENONE 0.25 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) STARCH, CORN (UNII: O8232NY3SJ) POVIDONE K25 (UNII: K0KQV10C35) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) Product Characteristics Color YELLOW Score no score Shape ROUND (biconvex) Size 6mm Flavor Imprint Code EL Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:50419-482-03 3 in 1 CARTON 02/29/2012 1 NDC:50419-482-01 28 in 1 BLISTER PACK; Type 0: Not a Combination Product 2 NDC:50419-482-72 1 in 1 CARTON 02/29/2012 2 NDC:50419-482-71 14 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021355 02/29/2012 Labeler - Bayer HealthCare Pharmaceuticals Inc. (005436809) Establishment Name Address ID/FEI Business Operations Bayer Weimar GmbH und Co. KG 331485631 MANUFACTURE(50419-483, 50419-482) , ANALYSIS(50419-483, 50419-482) Establishment Name Address ID/FEI Business Operations Bayer AG 314398484 API MANUFACTURE(50419-483, 50419-482) , ANALYSIS(50419-483, 50419-482) Establishment Name Address ID/FEI Business Operations Bayer AG 342872971 ANALYSIS(50419-483, 50419-482) , PARTICLE SIZE REDUCTION(50419-483, 50419-482) Establishment Name Address ID/FEI Business Operations Bayer AG 315097875 PACK(50419-483, 50419-482) , LABEL(50419-483, 50419-482) Establishment Name Address ID/FEI Business Operations Sharp Corporation 143696495 LABEL(50419-483, 50419-482)