Label: QUADRACEL- diphtheria and tetanus toxoids and acellular pertussis adsorbed and inactivated poliovirus vaccine injection, suspension
- NDC Code(s): 49281-564-10, 49281-564-15, 49281-564-58, 49281-564-88
- Packager: Sanofi Pasteur Inc.
- Category: VACCINE LABEL
- DEA Schedule: None
- Marketing Status: Biologic Licensing Application
Drug Label Information
Updated August 18, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Quadracel safely and effectively. See full prescribing information for Quadracel.
Quadracel (Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed and Inactivated Poliovirus Vaccine)
Suspension for Intramuscular Injection
Initial U.S. Approval: 2015INDICATIONS AND USAGE
Quadracel is a vaccine indicated for active immunization against diphtheria, tetanus, pertussis and poliomyelitis. A single dose of Quadracel is approved as a fifth dose in the diphtheria, tetanus, pertussis (DTaP) vaccination series, and as a fourth or fifth dose in the inactivated poliovirus (IPV) vaccination series in children 4 through 6 years of age whose previous DTaP vaccine doses have been with Pentacel, DAPTACEL and/or VAXELIS. (1)
DOSAGE AND ADMINISTRATION
A single intramuscular injection of 0.5 mL. (2)
DOSAGE FORMS AND STRENGTHS
Quadracel is a suspension for injection available in 0.5 mL single-dose vials and prefilled syringes. (3)
CONTRAINDICATIONS
- Severe allergic reaction (e.g., anaphylaxis) to any ingredient of Quadracel, or following any diphtheria toxoid, tetanus toxoid, pertussis-containing vaccine or inactivated poliovirus vaccine. (4.1) (11)
- Encephalopathy within 7 days of a previous pertussis-containing vaccine with no other identifiable cause. (4.2)
- Progressive neurologic disorder until a treatment regimen has been established and the condition has stabilized. (4.3)
WARNINGS AND PRECAUTIONS
- Carefully consider benefits and risks before administering Quadracel to persons with a history of:
- If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the decision to give any tetanus toxoid-containing vaccine, including Quadracel, should be based on careful consideration of the potential benefits and possible risks. (5.3)
ADVERSE REACTIONS
In a clinical study, the most common solicited injection site reactions were pain (>75%), increase in arm circumference (>65%), erythema (>55%), and swelling (>40%). Common solicited systemic reactions were myalgia (>50%), malaise (>35%), and headache (>15%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Pharmacovigilance Department, Sanofi Pasteur Inc., Discovery Drive, Swiftwater, PA 18370 at 1-800-822-2463 (1-800-VACCINE) or VAERS at 1-800-822-7967 or http://vaers.hhs.gov
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 8/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Encephalopathy
4.3 Progressive Neurologic Disorder
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
5.2 Adverse Reactions Following Prior Pertussis Vaccination
5.3 Guillain-Barré Syndrome
5.4 Limitations of Vaccine Effectiveness
5.5 Altered Immunocompetence
5.6 Syncope
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Concomitant Administration with Other Vaccines
7.2 Immunosuppressive Treatments
8 USE IN SPECIFIC POPULATIONS
8.4 Pediatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Immunogenicity
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Quadracel® is a vaccine indicated for active immunization against diphtheria, tetanus, pertussis and poliomyelitis. A single dose of Quadracel is approved for use as a fifth dose in the diphtheria, tetanus, pertussis (DTaP) vaccination series, and as a fourth or fifth dose in the inactivated poliovirus (IPV) vaccination series in children 4 through 6 years of age whose previous DTaP vaccine doses have been with Pentacel® [Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed, Inactivated Poliovirus and Haemophilus b conjugate (Tetanus Toxoid Conjugate) Vaccine], DAPTACEL® (Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed) and/or VAXELIS (Diphtheria and Tetanus Toxoids and Acellular Pertussis, Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B Vaccine).
-
2 DOSAGE AND ADMINISTRATION
For intramuscular injection only.
Just before use, shake the vial or syringe well, until a uniform, white, cloudy suspension results. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If either of these conditions exist, the product should not be administered.
Administer a 0.5 mL dose of Quadracel vaccine intramuscularly into the deltoid muscle of the upper arm. Discard unused portion in vial.
Quadracel should not be combined through reconstitution or mixed with any other vaccine.
-
3 DOSAGE FORMS AND STRENGTHS
Quadracel is a suspension for injection available in 0.5 mL single-dose vials and prefilled syringes [see How Supplied/Storage and Handling (16)].
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Severe allergic reaction (e.g., anaphylaxis) to any ingredient of Quadracel [see Description (11)] or following any diphtheria toxoid, tetanus toxoid, pertussis-containing vaccine, or inactivated poliovirus vaccine, is a contraindication to administration of Quadracel.
4.2 Encephalopathy
Encephalopathy (e.g., coma, decreased level of consciousness, prolonged seizures) within 7 days of a previous dose of a pertussis-containing vaccine that is not attributable to another identifiable cause is a contraindication to administration of any pertussis-containing vaccine, including Quadracel.
4.3 Progressive Neurologic Disorder
Progressive neurologic disorder, including infantile spasms, uncontrolled epilepsy, or progressive encephalopathy is a contraindication to administration of any pertussis-containing vaccine including Quadracel. Pertussis vaccine should not be administered to individuals with such conditions until a treatment regimen has been established and the condition has stabilized.
-
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Epinephrine hydrochloride solution (1:1,000) and other appropriate agents and equipment must be available for immediate use in case an anaphylactic or acute hypersensitivity reaction occurs.
5.2 Adverse Reactions Following Prior Pertussis Vaccination
If any of the following events have occurred within the specified period after administration of a pertussis vaccine, the decision to administer Quadracel should be based on careful consideration of benefits and risks.
- Temperature of ≥40.5°C (≥105°F) within 48 hours, not attributable to another identifiable cause.
- Collapse or shock-like state (hypotonic-hyporesponsive episode [HHE]) within 48 hours.
- Persistent, inconsolable crying lasting ≥3 hours within 48 hours.
- Seizures with or without fever within 3 days.
5.3 Guillain-Barré Syndrome
If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the decision to give any vaccine containing tetanus toxoid, including Quadracel, should be based on careful consideration of the potential benefits and possible risks.
5.4 Limitations of Vaccine Effectiveness
Vaccination with Quadracel may not protect all individuals.
5.5 Altered Immunocompetence
If Quadracel is administered to immunocompromised persons, including persons receiving immunosuppressive therapy, the expected immune response may not be obtained [see Drug Interactions (7.2)].
-
6 ADVERSE REACTIONS
In a clinical study, the most common solicited injection site reactions were pain (>75%), increase in arm circumference (>65%), erythema (>55%), and swelling (>40%). Common solicited systemic reactions were myalgia (>50%), malaise (>35%), and headache (>15%).
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to vaccine use and for approximating rates of those events. The poliovirus component (poliovirus types 1, 2, and 3) of this formulation of Quadracel is grown in Vero cells [see Description (11)]. The clinical study data in this section were accrued with a Quadracel formulation in which poliovirus component was grown in MRC-5 cells.
In a randomized, controlled, multicenter study conducted in the US and Puerto Rico (Study M5I02; ClinicalTrials.gov Identifier: NCT01346293), 3,372 children, 4 to 6 years of age, who had received 4 doses of DAPTACEL and/or Pentacel vaccine(s) received Quadracel, or DAPTACEL + IPOL (Poliovirus Vaccine Inactivated) vaccines administered concomitantly but at separate sites. Subjects also received Measles, Mumps, and Rubella Virus Vaccine Live (MMR) (Merck & Co., Inc.) and Varicella Virus Vaccine Live (Varicella vaccine) (Merck & Co., Inc.) administered concomitantly at separate sites. Safety was evaluated in 2,733 subjects who received Quadracel and 621 subjects who received DAPTACEL + IPOL vaccines.
Among these subjects, 51.5% were male, 48.5% were female, 75.7% were Caucasian, 8.6% were Black, 7.9% were Hispanic, 0.9% were Asian, and 7.8% were of other racial/ethnic groups. The mean age for both groups was 4.4 years and the ratio of male to female subjects and ethnicity were balanced between both groups.
Solicited injection site reactions and systemic reactions were collected daily for 7 days following vaccination, via diary cards. Participants were monitored for unsolicited adverse events for 28 days and serious adverse events (SAEs) for 6 months after vaccination.
Solicited Adverse Reactions
The incidence and severity of solicited injection site and systemic adverse reactions that occurred within 7 days after vaccination in each study group are shown in Table 1.
Table 1: Percentage of Children 4 through 6 years of Age with Solicited Adverse Reactions by Intensity Within 7 Days of Vaccination with Quadracel or Concomitant but Separate DAPTACEL and IPOL vaccines Co-Administered with MMR and Varicella Vaccines* Quadracel
(N†= 2,500-2,689)DAPTACEL + IPOL
(N† = 598-603)Injection Site Reactions Quadracel site DAPTACEL or IPOL site - *
- ClinicalTrials.gov Identifier: NCT01346293.
- †
- N = The number of subjects with available data.
- ‡
- Grade 1: Easily tolerated, Grade 2: Sufficiently discomforting to interfere with normal behavior or activities, Grade 3: Incapacitating, unable to perform usual activities.
- §
- Grade 1: >0 to <25 mm increase over pre-vaccination measurement, Grade 2: ≥25 to ≤50 mm increase over pre-vaccination measurement, Grade 3: >50 mm increase over pre-vaccination measurement.
- ¶
- Swelling of the injected limb including the adjacent joint (i.e., elbow and/or shoulder) as compared to baseline.
- #
- Grade 1: No interference with activity, Grade 2: Some interference with activity, Grade 3: Significant; prevents daily activity.
Pain‡, Any 77.4 76.5 Pain‡, Grade 1 56.4 54.9 Pain‡, Grade 2 19.0 18.6 Pain‡, Grade 3 2.0 3.0 Change in limb circumference§, Any 68.1 65.1 Change in limb circumference§, Grade 1 59.8 58.6 Change in limb circumference§, Grade 2 8.2 6.5 Change in limb circumference§, Grade 3 0.2 0.0 Erythema, Any 59.1 53.4 Erythema, >0 to <25 mm 31.6 31.8 Erythema, ≥25 to <50 mm 9.5 9.6 Erythema, ≥50 mm 18.0 11.9 Swelling, Any 40.2 36.4 Swelling, >0 to <25 mm 23.5 23.1 Swelling, ≥25 to <50 mm 8.1 6.1 Swelling, ≥50 mm 8.6 7.1 Extensive limb swelling¶, Any 1.5 1.3 Systemic Reactions Myalgia#, Any 53.8 52.6 Myalgia#, Grade 1 36.0 33.5 Myalgia#, Grade 2 15.8 16.3 Myalgia#, Grade 3 1.9 2.8 Malaise#, Any 35.0 33.2 Malaise#, Grade 1 21.7 18.7 Malaise#, Grade 2 10.6 11.1 Malaise#, Grade 3 2.6 3.3 Headache#, Any 15.6 16.6 Headache#, Grade 1 11.9 11.9 Headache#, Grade 2 3.1 4.0 Headache#, Grade 3 0.6 0.7 Fever, Any 6.0 6.9 Fever ≥38.0°C to ≤38.4°C 2.6 3.0 Fever, ≥38.5°C to ≤38.9°C 2.1 1.8 Fever, ≥39.0°C 1.3 2.0 Serious Adverse Events
In Study M5I02, within 28 days following vaccination with Quadracel, or DAPTACEL + IPOL vaccines, and concomitant MMR and varicella vaccines, 0.1% of subjects (3/2,733) in the Quadracel group experienced a serious adverse event. During the same time period, 0.2% subjects (1/621) in the DAPTACEL + IPOL group experienced a SAE. Within the 6-month follow-up period after vaccination, SAEs were reported in 0.8% of subjects (21/2,733) who received Quadracel and 0.5% of subjects (3/621) who received DAPTACEL + IPOL vaccines, none of which were assessed as related to vaccination.
6.2 Postmarketing Experience
The following adverse events have been spontaneously reported, during the post-marketing use of Quadracel outside the US, in infants and children from 2 months through 6 years of age. Because these events are reported voluntarily from a population of uncertain size, it is not possible to estimate their frequency reliably or establish a causal relationship to vaccine exposure. This list includes adverse events based on one or more of the following factors: severity, frequency of reporting, or strength of evidence for a causal relationship to Quadracel.
-
Immune system disorders
Anaphylactic reaction, hypersensitivity and allergic reactions (such as rash, urticaria, dyspnea) -
Psychiatric disorders
Screaming -
Nervous system disorders
Somnolence, convulsion, febrile convulsion, HHE, hypotonia -
Cardiac disorders
Cyanosis -
Vascular disorders
Pallor -
General disorders and administration site conditions
Listlessness
Injection site reactions (including inflammation, mass, sterile abscess, and edema)
Large injection site reactions (>50 mm), including limb swelling which may extend from the injection site beyond one or both joints -
Infections and Infestations
Injection site cellulitis, injection site abscess
-
7 DRUG INTERACTIONS
7.1 Concomitant Administration with Other Vaccines
In the US clinical trial, Study M5I02, Quadracel was administered concomitantly with one or more of the following US-licensed vaccines: MMR vaccine and varicella vaccine [see Adverse Reactions (6.1)].
When Quadracel is given at the same time as another injectable vaccine(s), the vaccines should be administered with different syringes and at different injection sites.
7.2 Immunosuppressive Treatments
Immunosuppressive therapies, including irradiation, antimetabolites, alkylating agents, cytotoxic drugs and corticosteroids (used in greater than physiologic doses), may reduce the immune response to Quadracel [see Warnings and Precautions (5.5)].
- 8 USE IN SPECIFIC POPULATIONS
-
11 DESCRIPTION
Quadracel (Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed and Inactivated Poliovirus Vaccine) is a sterile suspension for intramuscular injection.
Each 0.5 mL dose is formulated to contain 15 Lf diphtheria toxoid, 5 Lf tetanus toxoid, acellular pertussis antigens [20 mcg detoxified pertussis toxin (PT), 20 mcg filamentous hemagglutinin (FHA), 3 mcg pertactin (PRN), 5 mcg fimbriae types 2 and 3 (FIM)], and inactivated polioviruses [29 D-antigen units (DU) Type 1 (Mahoney), 7 DU Type 2 (MEF-1), 26 DU Type 3 (Saukett)].
Corynebacterium diphtheriae is grown in modified Mueller's growth medium. (1) After purification by ammonium sulfate fractionation, the diphtheria toxin is detoxified with formaldehyde and diafiltered.
Clostridium tetani is grown in modified Mueller-Miller casamino acid medium without beef heart infusion. (2) Tetanus toxin is detoxified with formaldehyde and purified by ammonium sulfate fractionation and diafiltration. Diphtheria and tetanus toxoids are individually adsorbed onto aluminum phosphate.
The acellular pertussis vaccine antigens are produced from Bordetella pertussis cultures grown in Stainer-Scholte medium (3) modified by the addition of casamino acids and dimethyl-beta-cyclodextrin. PT, FHA and PRN are isolated separately from the supernatant culture medium. FIM are extracted and copurified from the bacterial cells. The pertussis antigens are purified by sequential filtration, salt-precipitation, ultrafiltration and chromatography. PT is detoxified with glutaraldehyde. FHA is treated with formaldehyde and the residual aldehydes are removed by ultrafiltration. The individual antigens are adsorbed separately onto aluminum phosphate.
The Type 1, Type 2, and Type 3 polioviruses are individually grown in Vero cells (a continuous line of monkey kidney cells). Prior to viral propagation, the cells are grown in Iscove's medium, supplemented with calf serum. For viral propagation, the culture medium is replaced by M199 medium without calf serum. The viral harvests are concentrated and purified, then inactivated with formaldehyde to produce monovalent suspensions of each serotype. Specified quantities of monovalent suspensions of each serotype are mixed to produce the trivalent poliovirus concentrate. The adsorbed diphtheria, tetanus and acellular pertussis antigens are combined with aluminum phosphate, 2-phenoxyethanol (not as a preservative) and water for injection, into an intermediate concentrate. The trivalent poliovirus concentrate is added and the vaccine is diluted to its final concentration.
Each 0.5 mL dose contains 1.5 mg aluminum phosphate (0.33 mg aluminum) as the adjuvant, <8.1 mcg polysorbate 80, 3.3 mg (0.6% v/v) 2-phenoxyethanol (not as a preservative), 2 mcg to 7 mcg residual formaldehyde, <50 ng residual glutaraldehyde, ≤10 ng residual bovine serum albumin, <0.0001 pg streptomycin sulphate, <0.01 pg of neomycin and <0.000001 pg polymyxin B sulphate.
Quadracel does not contain a preservative.
Both diphtheria and tetanus toxoids induce at least 2 neutralizing units per mL in the guinea pig potency test. The potency of the acellular pertussis antigens is evaluated by the antibody response of immunized mice to detoxified PT, FHA, PRN and FIM as measured by enzyme-linked immunosorbent assay (ELISA). The potency of the inactivated poliovirus antigens is determined by measuring antibody-mediated neutralization of poliovirus in sera from immunized rats.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Diphtheria
Diphtheria is an acute toxin-mediated disease caused by toxigenic strains of C. diphtheriae. Protection against disease is due to the development of neutralizing antibodies to diphtheria toxin. A serum diphtheria antitoxin level of 0.01 IU/mL is the lowest level giving some degree of protection. Antitoxin levels of at least 0.1 IU/mL are generally regarded as protective. (4) Levels of 1.0 IU/mL have been associated with long-term protection. (5)
Tetanus
Tetanus is an acute disease caused by an extremely potent neurotoxin produced by C. tetani. Protection against disease is due to the development of neutralizing antibodies to tetanus toxin. A serum tetanus antitoxin level of at least 0.01 IU/mL, measured by neutralization assay, is considered the minimum protective level. (4) (6). A tetanus antitoxoid level ≥0.1 IU/mL as measured by the ELISA used in clinical studies of Quadracel is considered protective.
Pertussis
Pertussis (whooping cough) is a respiratory disease caused by B. pertussis. This Gram-negative coccobacillus produces a variety of biologically active components, though their role in either the pathogenesis of, or immunity to, pertussis has not been clearly defined.
There is no well-established serological correlate of protection for pertussis. Because DAPTACEL contains the same pertussis antigens manufactured by the same process as those in Quadracel, the effectiveness of Quadracel against pertussis was based on a comparison of pertussis immune responses following Quadracel to those following DAPTACEL (Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed) [see Clinical Studies (14)]. The efficacy of the pertussis component of DAPTACEL was determined in clinical trials of DAPTACEL administered to infants (see DAPTACEL prescribing information). Quadracel contains twice as much detoxified PT and four times as much FHA as DAPTACEL. Quadracel contains the same quantity of the same pertussis antigens manufactured by the same process as those in Pentacel and VAXELIS.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
The poliovirus component (poliovirus types 1, 2 and 3) of this formulation of Quadracel is grown in Vero cells [see Description (11)]. The clinical study data in this section were accrued with a Quadracel formulation in which the poliovirus component was grown in MRC-5 cells. The poliovirus component of the two formulations of Quadracel are analytically comparable.
14.1 Immunogenicity
In Study M5I02, children 4 through 6 years of age received Quadracel or DAPTACEL + IPOL as the fifth dose in the diphtheria, tetanus, and pertussis vaccination series and the fourth or fifth dose in the inactivated poliovirus vaccination series. Subjects also received their second dose of MMR and Varicella vaccines, concomitantly. The immunogenicity subset comprised 263 subjects in the Quadracel group and 253 subjects in the DAPTACEL + IPOL vaccines group [see Clinical Trials Experience (6.1)].
Antibody levels to diphtheria, tetanus, pertussis (PT, FHA, PRN and FIM) and poliovirus antigens were measured in sera obtained immediately prior to vaccination and 28 days after vaccination. The co-primary endpoints were booster response rates and antibody geometric mean concentrations/titers (GMCs/GMTs) to diphtheria, tetanus, pertussis and poliovirus antigens elicited after vaccination. Booster response rates and antibody GMCs/GMTs following Quadracel vaccination were compared to those after DAPTACEL + IPOL vaccination.
Quadracel was non-inferior to DAPTACEL + IPOL vaccines administered concomitantly at separate sites, as demonstrated by comparison of the post-vaccination antibody booster response rates and GMCs/GMTs to diphtheria and tetanus (Table 2), to all pertussis antigens (Table 3) and to poliovirus 1, 2 and 3 (Table 4).
Table 2: Booster Response Rates, Pre- and Post-Vaccination Seroprotection Rates and Post-Vaccination Antibody Levels to Diphtheria and Tetanus Antigens Following Quadracel or Concomitant but Separate DAPTACEL and IPOL Vaccines Co-Administered with MMR and Varicella Vaccines* Quadracel
(N†=253-262)DAPTACEL + IPOL
(N†=248-253)- *
- ClinicalTrials.gov Identifier: NCT01346293.
- †
- N = The number of subjects with available data.
- ‡
- Booster response: In subjects with pre-vaccination antibody concentrations <0.1 IU/mL, a post-vaccination level ≥0.4 IU/mL; in subjects with pre-vaccination antibody concentrations ≥0.1 IU/mL but <2.0 IU/mL, a 4-fold rise in post-vaccination level; in subjects with pre-vaccination antibody level ≥2.0 IU/mL, a 2-fold rise in post-vaccination level.
- §
- Quadracel was non-inferior to DAPTACEL + IPOL based on the post-vaccination booster response rates for diphtheria and tetanus (lower limits of the 2-sided 95% CIs of the difference [Quadracel minus DAPTACEL + IPOL] were >-10%).
- ¶
- Seroprotection: anti-diphtheria and anti-tetanus antibody concentrations ≥ 0.1 IU/mL and ≥ 1.0 IU/mL.
- #
- Quadracel was non-inferior to DAPTACEL + IPOL based on the post-vaccination GMCs for diphtheria and tetanus (lower limits of the 2-sided 95% CIs of the ratio [Quadracel / DAPTACEL + IPOL] were >2/3).
Anti-Diphtheria % Booster Response‡ 97.3§ 99.2 Pre-vaccination % ≥0.1 IU/mL¶ 90.7 83.1 Post-vaccination % ≥0.1 IU/mL¶ 100.0 99.6 Post-vaccination % ≥1.0 IU/mL¶ 99.6 99.6 Post-vaccination GMC (IU/mL) 18.6# 15.5 Anti-Tetanus % Booster Response‡ 84.2§ 84.3 Pre-vaccination % ≥0.1 IU/mL¶ 91.7 89.1 Post-vaccination % ≥0.1 IU/mL¶ 100.0 99.2 Post-vaccination % ≥1.0 IU/mL¶ 98.9 96.8 Post-vaccination GMC (IU/mL) 6.4# 5.5 Table 3: Booster Response Rates and Post-vaccination Antibody Levels to Pertussis Antigens Following Quadracel or Concomitant but Separate DAPTACEL and IPOL Vaccines Co-Administered with MMR and Varicella Vaccines* Quadracel
(N†=250-255)DAPTACEL + IPOL
(N†=247-249)- *
- ClinicalTrials.gov Identifier: NCT01346293.
- †
- N = The number of subjects with available data.
- ‡
- Booster response: In subjects with pre-vaccination antibody concentrations <LLOQ, a post-vaccination level ≥4×LLOQ; in subjects with pre-vaccination antibody concentrations ≥LLOQ but <4×LLOQ, a 4-fold rise in post-vaccination level; in subjects with pre-vaccination antibody level ≥4×LLOQ, a 2-fold rise in post-vaccination level.
- §
- Quadracel was non-inferior to DAPTACEL + IPOL based on the post-vaccination booster response rates for all pertussis antigens (lower limits of the 2-sided 95% CIs of the difference [Quadracel minus DAPTACEL + IPOL] were > -10%).
- ¶
- Quadracel was non-inferior to DAPTACEL + IPOL based on the post-vaccination GMCs for all pertussis antigens (lower limits of the 2-sided 95% CIs of the ratio [DTaP-IPV / DAPTACEL + IPOL] were >2/3).
Anti-PT % Booster Response‡ 95.2§ 89.9 Post-vaccination GMC (EU/mL) 120.7¶ 61.3 Anti-FHA % Booster Response‡ 94.9§ 87.5 Post-vaccination GMC (EU/mL) 123.5¶ 79.0 Anti-PRN % Booster Response‡ 96.9§ 93.1 Post-vaccination GMC (EU/mL) 282.6¶ 187.5 Anti-FIM % Booster Response‡ 97.2§ 92.4 Post-vaccination GMC (EU/mL) 505.8¶ 378.9 Table 4: Booster Response Rates, Pre- and Post-Vaccination Seroprotection Rates and Post-vaccination Antibody Levels to Poliovirus Antigens Following Quadracel or Concomitant but Separate DAPTACEL and IPOL Vaccines Co-Administered with MMR and Varicella Vaccines* Quadracel
(N†=247-258)DAPTACEL + IPOL
(N†=248-253)- *
- ClinicalTrials.gov Identifier: NCT01346293.
- †
- N = The number of subjects with available data.
- ‡
- Booster response: In subjects with pre-vaccination antibody concentrations <1:8 dilution, post-vaccination levels ≥1:8 dil; in subjects with pre-vaccination antibody concentrations ≥1:8 dilution, a 4-fold rise in post-vaccination antibody levels.
- §
- Quadracel was non-inferior to DAPTACEL + IPOL based on the post-vaccination booster response rates for polio types 1, 2 and 3 (lower limits of the 2-sided 95% CIs of the difference [Quadracel minus DAPTACEL + IPOL] were > -10%).
- ¶
- Quadracel was non-inferior to DAPTACEL + IPOL based on the post-vaccination GMTs for polio types 1, 2 and 3 (lower limits of the 2-sided 95% CIs of the ratio [Quadracel / DAPTACEL + IPOL] were >2/3).
Anti-Poliovirus 1 % Booster Response‡ 85.9§ 82.3 Pre-vaccination % ≥1:8 dilution 98.4 98.8 Post-vaccination % ≥1:8 dilution 100.0 99.6 Post-vaccination GMT 3,477¶ 2,731 Anti-Poliovirus 2 % Booster Response‡ 78.3§ 79.0 Pre-vaccination % ≥1:8 dilution 99.6 99.6 Post-vaccination % ≥1:8 dilution 100.0 100.0 Post-vaccination GMT 3,491¶ 3,894 Anti-Poliovirus 3 % Booster Response‡ 85.0§ 84.7 Pre-vaccination % ≥1:8 dilution 96.8 93.1 Post-vaccination % ≥1:8 dilution 100.0 100.0 Post-vaccination GMT 4,591¶ 3,419 -
15 REFERENCES
- 1
- Stainer DW. Production of diphtheria toxin. In: Manclark CR, editor. Proceedings of an informal consultation on the World Health Organization requirements for diphtheria, tetanus, pertussis and combined vaccines. United States Public Health Service, Bethesda, MD. DHHS 91-1174. 1991:7-11.
- 2
- Mueller JH, Miller PA. Variable factors influencing the production of tetanus toxin. J Bacteriol 1954;67(3):271-7.
- 3
- Stainer DW, Scholte MJ. A simple chemically defined medium for the production of phase I Bordetella pertussis. J Gen Microbiol 1970;63:211-20.
- 4
- Department of Health and Human Services, Food and Drug Administration. Biological products; bacterial vaccines and toxoids; implementation of efficacy review; proposed rule. Federal Register 1985;50(240):51002-117.
- 5
- Vitek CR, Tiwari TSP, Wharton M. Diphtheria toxoid. In: Plotkin SA, Orenstein WA, and Offit PA, editors. Vaccines. 7th ed. Philadelphia, PA: WB Saunders; 2018;7:261-75.
- 6
- Roper M, Wassilak SGF, Tiwari TSP, Orenstein WA. Tetanus toxoid. In: Plotkin SA, Orenstein WA, and Offit PA, editors. Vaccines. 7th ed. Philadelphia, PA: WB Saunders; 2018;18:1052-79.
- 7
- Sutter RW, et al. Defining surrogate serologic tests with respect to predicting protective vaccine efficacy: Poliovirus vaccination. In: Williams JC, et al. eds. Combined vaccines and simultaneous administration. Current issues and perspectives. New York, NY: The New York Academy of Sciences. 1995:289-99.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
The vial stopper, syringe plunger stopper, and syringe tip cap are not made with natural rubber latex.
Single-dose vial (NDC No. 49281-564-58) in packages of 10 vials (NDC No. 49281-564-10).
Single-dose, prefilled syringe, without needle, (NDC No. 49281-564-88). Supplied as package of 10 (NDC No. 49281-564-15).
-
17 PATIENT COUNSELING INFORMATION
Inform the parent or guardian of the following:
- The potential benefits and risks of immunization with Quadracel.
- The common adverse reactions that have occurred following administration of Quadracel or other vaccines containing similar components.
- Other adverse reactions can occur. Call healthcare provider with any adverse reactions of concern.
Provide the Vaccine Information Statements (VIS), which are required by the National Childhood Vaccine Injury Act of 1986.
- SPL UNCLASSIFIED SECTION
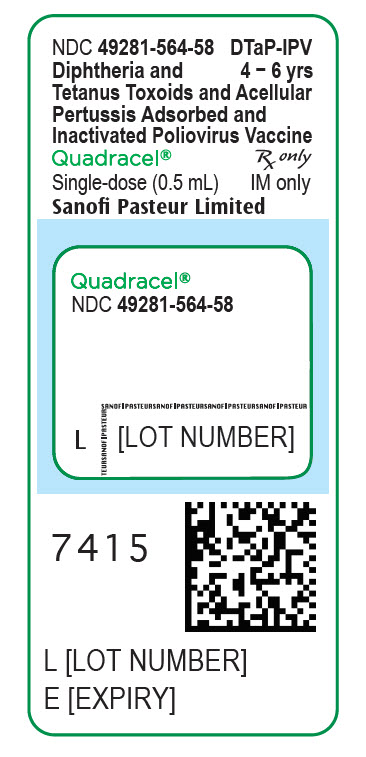
- PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Label
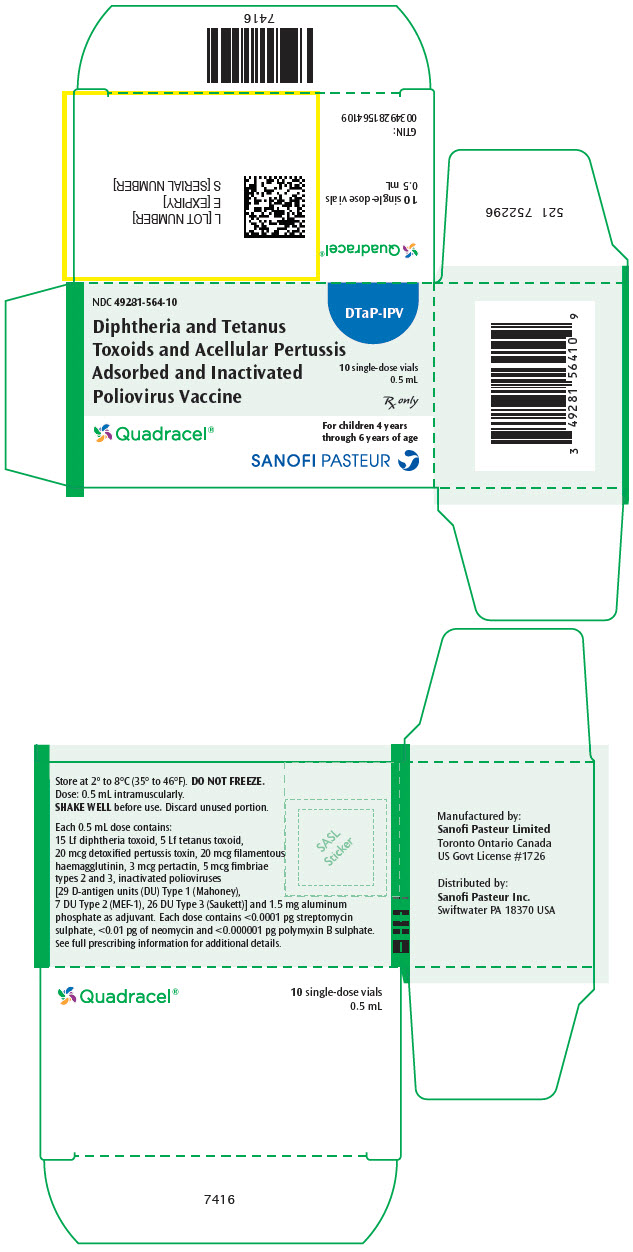
- PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Package
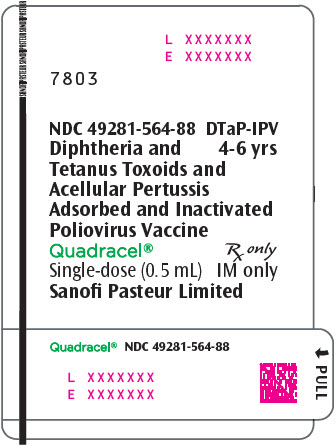
- PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Label
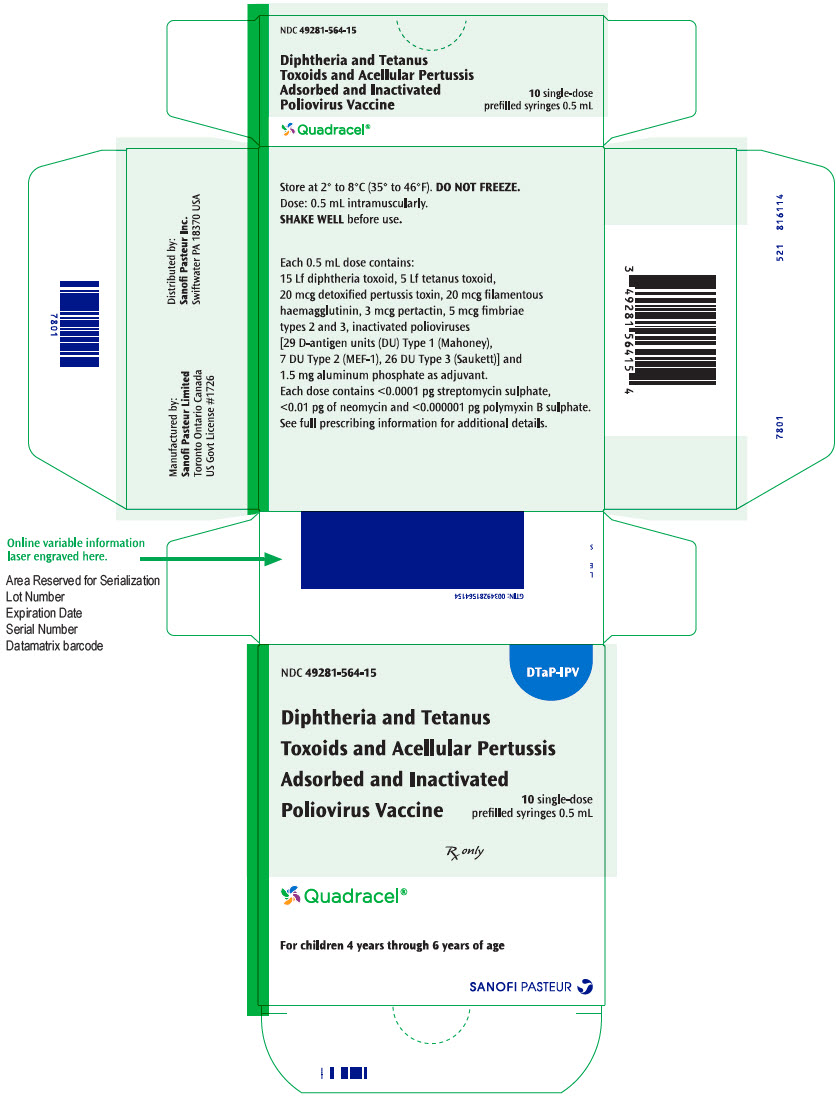
- PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Package
-
INGREDIENTS AND APPEARANCE
QUADRACEL
diphtheria and tetanus toxoids and acellular pertussis adsorbed and inactivated poliovirus vaccine injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC:49281-564 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: IRH51QN26H) (CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:IRH51QN26H) CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) 15 [Lf] in 0.5 mL CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: K3W1N8YP13) (CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:K3W1N8YP13) CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) 5 [Lf] in 0.5 mL BORDETELLA PERTUSSIS TOXOID ANTIGEN (GLUTARALDEHYDE INACTIVATED) (UNII: F4TN0IPY37) (BORDETELLA PERTUSSIS TOXOID ANTIGEN (GLUTARALDEHYDE INACTIVATED) - UNII:F4TN0IPY37) BORDETELLA PERTUSSIS TOXOID ANTIGEN (GLUTARALDEHYDE INACTIVATED) 20 ug in 0.5 mL BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 8C367IY4EY) (BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:8C367IY4EY) BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) 20 ug in 0.5 mL BORDETELLA PERTUSSIS PERTACTIN ANTIGEN (UNII: 63GD90PP8X) (BORDETELLA PERTUSSIS PERTACTIN ANTIGEN - UNII:63GD90PP8X) BORDETELLA PERTUSSIS PERTACTIN ANTIGEN 3 ug in 0.5 mL BORDETELLA PERTUSSIS FIMBRIAE 2/3 ANTIGEN (UNII: 1O0600285A) (BORDETELLA PERTUSSIS FIMBRIAE 2/3 ANTIGEN - UNII:1O0600285A) BORDETELLA PERTUSSIS FIMBRIAE 2/3 ANTIGEN 5 ug in 0.5 mL POLIOVIRUS TYPE 1 ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 0LVY784C09) (POLIOVIRUS TYPE 1 ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:0LVY784C09) POLIOVIRUS TYPE 1 ANTIGEN (FORMALDEHYDE INACTIVATED) 29 [D'ag'U] in 0.5 mL POLIOVIRUS TYPE 2 ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 23JE9KDF4R) (POLIOVIRUS TYPE 2 ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:23JE9KDF4R) POLIOVIRUS TYPE 2 ANTIGEN (FORMALDEHYDE INACTIVATED) 7 [D'ag'U] in 0.5 mL POLIOVIRUS TYPE 3 ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 459ROM8M9M) (POLIOVIRUS TYPE 3 ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:459ROM8M9M) POLIOVIRUS TYPE 3 ANTIGEN (FORMALDEHYDE INACTIVATED) 26 [D'ag'U] in 0.5 mL Inactive Ingredients Ingredient Name Strength ALUMINUM PHOSPHATE (UNII: F92V3S521O) 1.5 mg in 0.5 mL PHENOXYETHANOL (UNII: HIE492ZZ3T) 3.3 mg in 0.5 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) FORMALDEHYDE (UNII: 1HG84L3525) GLUTARAL (UNII: T3C89M417N) ALBUMIN BOVINE (UNII: 27432CM55Q) STREPTOMYCIN SULFATE (UNII: CW25IKJ202) NEOMYCIN (UNII: I16QD7X297) POLYMYXIN B SULFATE (UNII: 19371312D4) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE (WHITE TO OFF-WHITE) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:49281-564-10 10 in 1 PACKAGE 1 NDC:49281-564-58 0.5 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product 2 NDC:49281-564-15 10 in 1 PACKAGE 2 NDC:49281-564-88 0.5 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125525 03/24/2015 Labeler - Sanofi Pasteur Inc. (086723285) Establishment Name Address ID/FEI Business Operations Sanofi Pasteur Limited 208206623 MANUFACTURE