Label: AZITHROMYCIN- azithromycin monohydrate injection, powder, lyophilized, for solution
- NDC Code(s): 63323-398-14, 63323-398-41
- Packager: Fresenius Kabi USA, LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated October 11, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Azithromycin for Injection, USP safely and effectively.
See full prescribing information for Azithromycin for Injection, USP.
Azithromycin for Injection, USP, for intravenous use
Initial U.S. Approval: 1991INDICATIONS AND USAGE
Azithromycin for injection, USP is a macrolide antibacterial drug indicated for mild to moderate infections caused by designated, susceptible bacteria:
To reduce the development of drug-resistant bacteria and maintain the effectiveness of azithromycin for injection, USP and other antibacterial drugs, azithromycin for injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria.
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
- Azithromycin for injection is supplied in lyophilized form in a 10 mL vial equivalent to 500 mg of azithromycin for intravenous administration. ( 3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Serious (including fatal) allergic reactions and skin reactions. Discontinue azithromycin and initiate appropriate therapy if reaction occurs. ( 5.1)
- Hepatotoxicity: Severe and sometimes fatal, hepatoxicity has been reported. Discontinue azithromycin immediately if signs and symptoms of hepatitis occur. ( 5.2)
- Infantile Hypertrophic Pyloric Stenosis (IHPS): Following the use of azithromycin in neonates (treatment up to 42 days of life), IHPS has been reported. Direct parents and caregivers to contact their physician if vomiting or irritability with feeding occurs. ( 5.3)
- Prolongation of QT interval and cases of torsades de pointes have been reported. This risk which can be fatal should be considered in patients with certain cardiovascular disorders including known QT prolongation or history torsades de pointes, those with proarrhythmic conditions, and with other drugs that prolong the QT interval. ( 5.4)
- Clostridium difficile-Associated Diarrhea: Evaluate patients if diarrhea occurs. ( 5.5)
- Azithromycin may exacerbate muscle weakness in persons with myasthenia gravis. ( 5.6)
ADVERSE REACTIONS
Most common adverse reactions are nausea (4%), diarrhea (4%), abdominal pain (3%), or vomiting (1%). ( 6)
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC, at 1-800-551-7176 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 9/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Community-Acquired Pneumonia
1.2 Pelvic Inflammatory Disease
1.3 Usage
2 DOSAGE AND ADMINISTRATION
2.1 Community-Acquired Pneumonia
2.2 Pelvic Inflammatory Disease
2.3 Preparation of the Solution for Intravenous Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Hepatic Dysfunction
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
5.2 Hepatotoxicity
5.3 Infantile Hypertrophic Pyloric Stenosis (IHPS)
5.4 QT Prolongation
5.5 Clostridium Difficile-Associated Diarrhea
5.6 Exacerbation of Myasthenia Gravis
5.7 Infusion Site Reactions
5.8 Development of Drug-Resistant Bacteria
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
6.3 Laboratory Abnormalities
7 DRUG INTERACTIONS
7.1 Nelfinavir
7.2 Warfarin
7.3 Potential Drug-Drug Interaction with Macrolides
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Community-Acquired Pneumonia
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Azithromycin for injection is a macrolide antibacterial drug indicated for the treatment of patients with infections caused by susceptible strains of the designated microorganisms in the conditions listed below.
1.1 Community-Acquired Pneumonia
due to Chlamydophila pneumoniae, Haemophilus influenzae, Legionella pneumophila, Moraxella catarrhalis, Mycoplasma pneumoniae, Staphylococcus aureus, or Streptococcus pneumoniae in patients who require initial intravenous therapy.
1.2 Pelvic Inflammatory Disease
due to Chlamydia trachomatis, Neisseria gonorrhoeae, or Mycoplasma hominis in patients who require initial intravenous therapy. If anaerobic microorganisms are suspected of contributing to the infection, an antimicrobial agent with anaerobic activity should be administered in combination with Azithromycin for injection.
Azithromycin for injection should be followed by Azithromycin by the oral route as required. [see Dosage and Administration ( 2)]
1.3 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Azithromycin and other antibacterial drugs, Azithromycin should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
-
2 DOSAGE AND ADMINISTRATION
[see Indications and Usage ( 1) and Clinical Pharmacology ( 12.3)]
2.1 Community-Acquired Pneumonia
The recommended dose of azithromycin for injection for the treatment of adult patients with community-acquired pneumonia due to the indicated organisms is 500 mg as a single daily dose by the intravenous route for at least two days. Intravenous therapy should be followed by azithromycin by the oral route at a single, daily dose of 500 mg, administered as two 250 mg tablets to complete a 7- to 10-day course of therapy. The timing of the switch to oral therapy should be done at the discretion of the physician and in accordance with clinical response.
2.2 Pelvic Inflammatory Disease
The recommended dose of azithromycin for injection for the treatment of adult patients with pelvic inflammatory disease due to the indicated organisms is 500 mg as a single daily dose by the intravenous route for one or two days. Intravenous therapy should be followed by azithromycin by the oral route at a single, daily dose of 250 mg to complete a 7-day course of therapy. The timing of the switch to oral therapy should be done at the discretion of the physician and in accordance with clinical response.
2.3 Preparation of the Solution for Intravenous Administration
The infusate concentration and rate of infusion for azithromycin for injection should be either 1 mg/mL over 3 hr or 2 mg/mL over 1 hr. Azithromycin for injection should not be given as a bolus or as an intramuscular injection.
Reconstitution
Prepare the initial solution of azithromycin for injection by adding 4.8 mL of Sterile Water for Injection to the 500 mg vial, and shaking the vial until all of the drug is dissolved. Since azithromycin for injection is supplied under vacuum, it is recommended that a standard 5 mL (non-automated) syringe be used to ensure that the exact amount of 4.8 mL of Sterile Water is dispensed. Each mL of reconstituted solution contains 100 mg azithromycin. Reconstituted solution is stable for 24 hr when stored below 30°C (86°F).
Parenteral drug products should be inspected visually for particulate matter prior to administration. If particulate matter is evident in reconstituted fluids, the drug solution should be discarded.
Dilute this solution further prior to administration as instructed below.
Dilution
To provide azithromycin over a concentration range of 1.0-2.0 mg/mL, transfer 5 mL of the 100 mg/mL azithromycin solution into the appropriate amount of any of the diluents listed below:
Normal Saline (0.9% sodium chloride)
1/2 Normal Saline (0.45% sodium chloride)
5% Dextrose in Water
Lactated Ringer's Solution
5% Dextrose in 1/2 Normal Saline (0.45% sodium chloride) with 20 mEq KCl
5% Dextrose in Lactated Ringer's Solution
5% Dextrose in 1/3 Normal Saline (0.3% sodium chloride)
5% Dextrose in 1/2 Normal Saline (0.45% sodium chloride)
Normosol ®-M in 5% Dextrose
Normosol ®-R in 5% Dextrose
When used with the Vial-Mate ® drug reconstitution device, please reference the Vial-Mate ® instructions for assembly and reconstitution.
Final Infusion Solution Concentration (mg/mL) Amount of Diluent (mL) 1.0 mg/mL 500 mL 2.0 mg/mL 250 mL Other intravenous substances, additives, or medications should not be added to azithromycin for injection, or infused simultaneously through the same intravenous line.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
Serious allergic reactions, including angioedema, anaphylaxis, and dermatologic reactions including Acute Generalized Exanthematous Pustulosis (AGEP), Stevens-Johnson Syndrome, and toxic epidermal necrolysis have been reported in patients on azithromycin therapy [see Contraindications ( 4.1)].
Fatalities have been reported. Cases of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) have also been reported. Despite initially successful symptomatic treatment of the allergic symptoms, when symptomatic therapy was discontinued, the allergic symptoms recurred soon thereafter in some patients without further azithromycin exposure. These patients required prolonged periods of observation and symptomatic treatment. The relationship of these episodes to the long tissue half-life of azithromycin and subsequent prolonged exposure to antigen is unknown at present.
If an allergic reaction occurs, the drug should be discontinued and appropriate therapy should be instituted. Physicians should be aware that the allergic symptoms may reappear after symptomatic therapy has been discontinued.
5.2 Hepatotoxicity
Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure have been reported, some of which have resulted in death. Discontinue azithromycin immediately if signs and symptoms of hepatitis occur.
5.3 Infantile Hypertrophic Pyloric Stenosis (IHPS)
Following the use of azithromycin in neonates (treatment up to 42 days of life), IHPS has been reported. Direct parents and caregivers to contact their physician if vomiting or irritability with feeding occurs.
5.4 QT Prolongation
Prolonged cardiac repolarization and QT interval, imparting a risk of developing cardiac arrhythmia and torsades de pointes, have been seen with treatment with macrolides, including azithromycin. Cases of torsades de pointes have been spontaneously reported during postmarketing surveillance in patients receiving azithromycin. Providers should consider the risk of QT prolongation, which can be fatal when weighing the risks and benefits of azithromycin for at-risk groups including:
- patients with known prolongation of the QT interval, a history of torsades de pointes, congenital long QT syndrome, bradyarrhythmias or uncompensated heart failure
- patients on drugs known to prolong the QT interval
- patients with ongoing proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, and in patients receiving Class IA (quinidine, procainamide) or Class III (dofetilide, amiodarone, sotalol) antiarrhythmic agents.
Elderly patients may be more susceptible to drug-associated effects on the QT interval.
5.5 Clostridium Difficile-Associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including azithromycin for injection, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antibacterial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.6 Exacerbation of Myasthenia Gravis
Exacerbations of symptoms of myasthenia gravis and new onset of myasthenic syndrome have been reported in patients receiving azithromycin therapy.
5.7 Infusion Site Reactions
Azithromycin for injection should be reconstituted and diluted as directed and administered as an intravenous infusion over not less than 60 minutes [see Dosage and Administration ( 2)].
Local IV site reactions have been reported with the intravenous administration of azithromycin. The incidence and severity of these reactions were the same when 500 mg azithromycin was given over 1 hour (2 mg/mL as 250 mL infusion) or over 3 hr (1 mg/mL as 500 mL infusion) [see Adverse Reactions ( 6)]. All volunteers who received infusate concentrations above 2 mg/mL experienced local IV site reactions and, therefore, higher concentrations should be avoided.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials of intravenous azithromycin for community-acquired pneumonia, in which 2 to 5 IV doses were given, the reported adverse reactions were mild to moderate in severity and were reversible upon discontinuation of the drug. The majority of patients in these trials had one or more co-morbid diseases and were receiving concomitant medications. Approximately 1.2% of the patients discontinued intravenous azithromycin therapy, and a total of 2.4% discontinued azithromycin therapy by either the intravenous or oral route because of clinical or laboratory side effects.
In clinical trials conducted in patients with pelvic inflammatory disease, in which 1 to 2 IV doses were given, 2% of women who received monotherapy with azithromycin and 4% who received azithromycin plus metronidazole discontinued therapy due to clinical side effects.
Clinical adverse reactions leading to discontinuations from these studies were gastrointestinal (abdominal pain, nausea, vomiting, diarrhea), and rashes; laboratory side effects leading to discontinuation were increases in transaminase levels and/or alkaline phosphatase levels.
Overall, the most common adverse reactions associated with treatment in adult patients who received IV/Oral azithromycin in studies of community-acquired pneumonia were related to the gastrointestinal system with diarrhea/loose stools (4.3%), nausea (3.9%), abdominal pain (2.7%), and vomiting (1.4%) being the most frequently reported.
Approximately 12% of patients experienced a side effect related to the intravenous infusion; most common were pain at the injection site (6.5%) and local inflammation (3.1%).
The most common adverse reactions associated with treatment in adult women who received IV/Oral azithromycin in trials of pelvic inflammatory disease were related to the gastrointestinal system. Diarrhea (8.5%) and nausea (6.6%) were most commonly reported, followed by vaginitis (2.8%), abdominal pain (1.9%), anorexia (1.9%), rash and pruritus (1.9%). When azithromycin was co-administered with metronidazole in these trials, a higher proportion of women experienced adverse reactions of nausea (10.3%), abdominal pain (3.7%), vomiting (2.8%), infusion site reaction, stomatitis, dizziness, or dyspnea (all at 1.9%).
Adverse reactions that occurred with a frequency of 1% or less included the following:
Gastrointestinal: Dyspepsia, flatulence, mucositis, oral moniliasis, and gastritis.
Nervous system: Headache, somnolence.
Allergic: Bronchospasm.
Special senses: Taste perversion.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of azithromycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse reactions reported with azithromycin during the postmarketing period in adult and/or pediatric patients for which a causal relationship may not be established include:
Allergic: Arthralgia, edema, urticaria and angioedema.
Cardiovascular: Arrhythmias including ventricular tachycardia and hypotension. There have been reports of QT prolongation and torsades de pointes.
Gastrointestinal: Anorexia, constipation, dyspepsia, flatulence, vomiting/diarrhea, pseudomembranous colitis, pancreatitis, oral candidiasis, pyloric stenosis, and reports of tongue discoloration.
General: Asthenia, paresthesia, fatigue, malaise and anaphylaxis (including fatalities).
Genitourinary: Interstitial nephritis and acute renal failure and vaginitis.
Hematopoietic: Thrombocytopenia.
Liver/biliary: Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure [see Warnings and Precautions ( 5.2)].
Nervous system: Convulsions, dizziness/vertigo, headache, somnolence, hyperactivity, nervousness, agitation and syncope.
Psychiatric: Aggressive reaction and anxiety.
Skin/appendages: Pruritus, serious skin reactions including, erythema multiforme, AGEP, Stevens-Johnson syndrome, toxic epidermal necrolysis, and DRESS.
Special senses: Hearing disturbances including hearing loss, deafness and/or tinnitus and reports of taste/smell perversion and/or loss.
6.3 Laboratory Abnormalities
Significant abnormalities (irrespective of drug relationship) occurring during the clinical trials were reported as follows:
- elevated ALT (SGPT), AST (SGOT), creatinine (4 to 6%)
- elevated LDH, bilirubin (1 to 3%)
- leukopenia, neutropenia, decreased platelet count, and elevated serum alkaline phosphatase (less than 1%)
When follow-up was provided, changes in laboratory tests appeared to be reversible.
In multiple-dose clinical trials involving more than 750 patients treated with azithromycin (IV/Oral), less than 2% of patients discontinued azithromycin therapy because of treatment-related liver enzyme abnormalities.
-
7 DRUG INTERACTIONS
7.1 Nelfinavir
Co-administration of nelfinavir at steady-state with a single oral dose of azithromycin resulted in increased azithromycin serum concentrations. Although a dose adjustment of azithromycin is not recommended when administered in combination with nelfinavir, close monitoring for known adverse reactions of azithromycin, such as liver enzyme abnormalities and hearing impairment, is warranted [see Adverse Reactions ( 6)].
7.2 Warfarin
Spontaneous postmarketing reports suggest that concomitant administration of azithromycin may potentiate the effects of oral anticoagulants such as warfarin, although the prothrombin time was not affected in the dedicated drug interaction study with azithromycin and warfarin. Prothrombin times should be carefully monitored while patients are receiving azithromycin and oral anticoagulants concomitantly.
7.3 Potential Drug-Drug Interaction with Macrolides
Interactions with digoxin, colchicine or phenytoin have not been reported in clinical trials with azithromycin. No specific drug interaction studies have been performed to evaluate potential drug-drug interaction. However, drug interactions have been observed with other macrolide products. Until further data are developed regarding drug interactions when digoxin, colchicine or phenytoin are used with azithromycin careful monitoring of patients is advised.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from published literature and postmarketing experience over several decades with azithromycin use in pregnant women have not identified any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data).
Developmental toxicity studies with azithromycin in rats, mice, and rabbits showed no drug-induced fetal malformations at doses up to 4, 2, and 2 times, respectively, an adult human daily dose of 500 mg based on body surface area. Decreased viability and delayed development were observed in the offspring of pregnant rats administered azithromycin from day 6 of pregnancy through weaning at a dose equivalent to 4 times an adult human daily dose of 500 mg based on body surface area (see Data) .
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
Available data from published observational studies, case series, and case reports over several decades do not suggest an increased risk for major birth defects, miscarriage, or adverse maternal or fetal outcomes with azithromycin use in pregnant women. Limitations of these data include the lack of randomization and inability to control for confounders such as underlying maternal disease and maternal use of concomitant medications.
Animal Data
Reproductive and developmental toxicology studies have not been conducted using IV administration of azithromycin to animals. Azithromycin administered during the period of organogenesis did not cause fetal malformations in rats and mice at oral doses up to 200 mg/kg/day (moderately maternally toxic). Based on body surface area, this dose is approximately 4 (rats) and 2 (mice) times an adult human daily dose of 500 mg. In rabbits administered azithromycin at oral doses of 10, 20, and 40 mg/kg/day during organogenesis, reduced maternal body weight and food consumption were observed in all groups; no evidence of fetotoxicity or teratogenicity was observed at these doses, the highest of which is estimated to be 2 times an adult human daily dose of 500 mg based on body surface area.
In a pre- and postnatal development study, azithromycin was administered orally to pregnant rats from day 6 of pregnancy until weaning at doses of 50 or 200 mg/kg/day. Maternal toxicity (reduced food consumption and body weight gain; increased stress at parturition) was observed at the higher dose. Effects in the offspring were noted at 200 mg/kg/day during the postnatal development period (decreased viability, delayed developmental landmarks). These effects were not observed in a pre- and postnatal rat study when up to 200 mg/kg/day of azithromycin was given orally beginning on day 15 of pregnancy until weaning
8.2 Lactation
Risk Summary
Azithromycin is present in human milk (see Data) . Non-serious adverse reactions have been reported in breastfed infants after maternal administration of azithromycin (see Clinical Considerations) . There are no available data on the effects of azithromycin on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for azithromycin and any potential adverse effects on the breastfed infant from azithromycin or from the underlying maternal condition.
Clinical Considerations
Advise women to monitor the breastfed infant for diarrhea, vomiting, or rash.
Data
Azithromycin breastmilk concentrations were measured in 20 women after receiving a single 2 g oral dose of azithromycin during labor. Breastmilk samples collected on days 3 and 6 postpartum as well as 2 and 4 weeks postpartum revealed the presence of azithromycin in breastmilk up to 4 weeks after dosing. In another study, a single dose of azithromycin 500 mg was administered intravenously to 8 women prior to incision for cesarean section. Breastmilk (colostrum) samples obtained between 12 and 48 hours after dosing revealed that azithromycin persisted in breastmilk up to 48 hours.
8.4 Pediatric Use
Safety and effectiveness of azithromycin for injection in children or adolescents under 16 years have not been established. In controlled clinical studies, azithromycin has been administered to pediatric patients (age 6 months to 16 years) by the oral route. For information regarding the use of azithromycin for oral suspension in the treatment of pediatric patients, [see Indications and Usage ( 1), and Dosage and Administration ( 2)] of the prescribing information for azithromycin for oral suspension 100 mg/5 mL and 200 mg/5 mL bottles.
8.5 Geriatric Use
Pharmacokinetic studies with intravenous azithromycin have not been performed in older volunteers. Pharmacokinetics of azithromycin following oral administration in older volunteers (65 to 85 years old) were similar to those in younger volunteers (18 to 40 years old) for the 5-day therapeutic regimen.
In multiple-dose clinical trials of intravenous azithromycin in the treatment of community-acquired pneumonia, 45% of patients (188/414) were at least 65 years of age and 22% of patients (91/414) were at least 75 years of age. No overall differences in safety were observed between these subjects and younger subjects in terms of adverse reactions, laboratory abnormalities, and discontinuations. Similar decreases in clinical response were noted in azithromycin- and comparator-treated patients with increasing age.
Azithromycin for injection contains 114 mg (4.96 mEq) of sodium per vial. At the usual recommended doses, patients would receive 114 mg (4.96 mEq) of sodium. The geriatric population may respond with a blunted natriuresis to salt loading. The total sodium content from dietary and non-dietary sources may be clinically important with regard to such diseases as congestive heart failure.
Elderly patients may be more susceptible to development of torsades de pointes arrhythmias than younger patients [see Warnings and Precautions ( 5.4)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
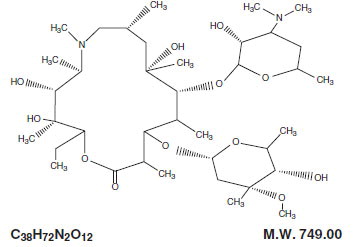
Azithromycin for injection, USP contains the active ingredient azithromycin, an azalide, a subclass of macrolide antibacterial drug, for intravenous injection. Azithromycin has the chemical name (2R,3S,4R,5R,8R,10R,11R,12S,13S,14R)-13-[(2,6-dideoxy-3- C-methyl-3- O-methyl-α- L-ribo-hexopyranosyl)oxy]-2-ethyl-3,4,10-trihydroxy-3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β- D- xylo-hexopyranosyl]oxy]-1-oxa-6-azacyclopentadecan-15-one. Azithromycin is derived from erythromycin; however, it differs chemically from erythromycin in that a methyl-substituted nitrogen atom is incorporated into the lactone ring. Its molecular formula is C 38 H 72 N 2 O 12, and its molecular weight is 749.00. Azithromycin has the following structural formula:
Azithromycin, as the monohydrate or dihydrate, is a white crystalline powder with a molecular formula of C 38H 72N 2O 12•H 2O or C 38H 72N 2O 12•2H 2O and a molecular weight of 767.00 or 785.02 respectively.
Azithromycin for injection, USP consists of azithromycin monohydrate or dihydrate and the following inactive ingredients: citric acid and sodium hydroxide. Azithromycin for injection, USP is supplied in lyophilized form in a 10 mL vial equivalent to 500 mg of azithromycin for intravenous administration. Reconstitution, according to label directions, results in approximately 5 mL of azithromycin for intravenous injection with each mL containing azithromycin monohydrate or dihydrate equivalent to 100 mg of azithromycin.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
Based on animal models of infection, the antibacterial activity of azithromycin appears to correlate with the ratio of area under the concentration-time curve to minimum inhibitory concentration (AUC/MIC) for certain pathogens ( S. pneumoniae and S. aureus). The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and microbiological cure has not been elucidated in clinical trials with azithromycin.
Cardiac Electrophysiology
QTc interval prolongation was studied in a randomized, placebo-controlled parallel trial in 116 healthy subjects who received either chloroquine (1,000 mg) alone or in combination with oral azithromycin (500 mg, 1,000 mg, and 1,500 mg once daily). Co-administration of azithromycin increased the QTc interval in a dose- and concentration-dependent manner. In comparison to chloroquine alone, the maximum mean (95% upper confidence bound) increases in QTcF were 5 (10) ms, 7 (12) ms and 9 (14) ms with the co-administration of 500 mg, 1,000 mg and 1,500 mg azithromycin, respectively.
Since the mean C max of azithromycin following a 500 mg IV dose given over 1 hour is higher than the mean C max of azithromycin following the administration of a 1,500 mg oral dose, it is possible that QTc may be prolonged to a greater extent with IV azithromycin at close proximity to a one hour infusion of 500 mg.
12.3 Pharmacokinetics
In patients hospitalized with community-acquired pneumonia receiving single daily one-hour intravenous infusions for 2 to 5 days of 500 mg azithromycin at a concentration of 2 mg/mL, the mean C max ± S.D. achieved was 3.63 ± 1.60 mcg/mL, while the 24-hour trough level was 0.20 ± 0.15 mcg/mL, and the AUC 24 was 9.60 ± 4.80 mcg•hr/mL.
The mean C max , 24-hour trough and AUC 24 values were 1.14 ± 0.14 mcg/mL, 0.18 ± 0.02 mcg/mL, and 8.03 ±0.86 mcg•hr/mL, respectively, in normal volunteers receiving a 3-hour intravenous infusion of 500 mg azithromycin at a concentration of 1 mg/mL. Similar pharmacokinetic values were obtained in patients hospitalized with community-acquired pneumonia who received the same 3-hour dosage regimen for 2-5 days.
a500 mg (2 mg/mL) for 2-5 days in community-acquired pneumonia patients.
b500 mg (1 mg/mL) for 5 days in healthy subjects.
Infusion Concentration, Duration Time after starting the infusion (hr) 0.5 1 2 3 4 6 8 12 24 2 mg/mL,
1 hra2.98 ± 1.12 3.63 ± 1.73 0.60 ± 0.31 0.40 ± 0.23 0.33 ± 0.16 0.26 ± 0.14 0.27 ± 0.15 0.20 ± 0.12 0.20 ± 0.15 1 mg/mL,
3 hrb0.91 ± 0.13 1.02 ± 0.11 1.14 ± 0.13 1.13 ± 0.16 0.32 ± 0.05 0.28 ± 0.04 0.27 ± 0.03 0.22 ± 0.02 0.18 ± 0.02 Comparison of the plasma pharmacokinetic parameters following the 1st and 5th daily doses of 500 mg intravenous azithromycin showed only an 8% increase in C max but a 61% increase in AUC 24 reflecting a threefold rise in C 24 trough levels.
Following single-oral doses of 500 mg azithromycin (two 250 mg capsules) to 12 healthy volunteers, C max, trough level, and AUC 24 were reported to be 0.41 mcg/mL, 0.05 mcg/mL, and 2.6 mcg•h/mL, respectively. These oral values are approximately 38%, 83%, and 52% of the values observed following a single 500 mg I.V. 3-hour infusion (C max,: 1.08 mcg/mL, trough: 0.06 mcg/mL, and AUC 24: 5 mcg•h/mL). Thus, plasma concentrations are higher following the intravenous regimen throughout the 24-hour interval.
Distribution
The serum protein binding of azithromycin is variable in the concentration range approximating human exposure, decreasing from 51% at 0.02 mcg/mL to 7% at 2 mcg/mL.
Tissue concentrations have not been obtained following intravenous infusions of azithromycin, but following oral administration in humans azithromycin has been shown to penetrate into tissues, including skin, lung, tonsil, and cervix.
Tissue levels were determined following a single oral dose of 500 mg azithromycin in 7 gynecological patients. Approximately 17 hr after dosing, azithromycin concentrations were 2.7 mcg/g in ovarian tissue, 3.5 mcg/g in uterine tissue, and 3.3 mcg/g in salpinx. Following a regimen of 500 mg on the first day followed by 250 mg daily for 4 days, concentrations in the cerebrospinal fluid were less than 0.01 mcg/mL in the presence of non-inflamed meninges.
Metabolism
In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed.
Elimination
Plasma concentrations of azithromycin following single 500 mg oral and IV doses declined in a polyphasic pattern with a mean apparent plasma clearance of 630 mL/min and terminal elimination half-life of 68 hours. The prolonged terminal half-life is thought to be due to extensive uptake and subsequent release of drug from tissues.
In a multiple-dose study in 12 normal volunteers utilizing a 500 mg (1 mg/mL) one-hour intravenous-dosage regimen for five days, the amount of administered azithromycin dose excreted in urine in 24 hours was about 11% after the 1st dose and 14% after the 5th dose. These values are greater than the reported 6% excreted unchanged in urine after oral administration of azithromycin. Biliary excretion is a major route of elimination for unchanged drug, following oral administration.
Specific Populations
Patients with Renal Impairment
Azithromycin pharmacokinetics were investigated in 42 adults (21 to 85 years of age) with varying degrees of renal impairment. Following the oral administration of a single 1,000 mg dose of azithromycin, mean C max and AUC 0-120 increased by 5.1% and 4.2%, respectively in subjects with mild to moderate renal impairment (GFR 10 to 80 mL/min) compared to subjects with normal renal function (GFR > 80 mL/min). The mean C max and AUC 0-120 increased 61% and 35%, respectively in subjects with severe renal impairment (GFR < 10 mL/min) compared to subjects with normal renal function (GFR > 80 mL/min).
Patients with Hepatic Impairment
The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been established.
Male and Female Patients
There are no significant differences in the disposition of azithromycin between male and female subjects. No dosage adjustment is recommended based on gender.
Geriatric Patients
Pharmacokinetic studies with intravenous azithromycin have not been performed in older volunteers. Pharmacokinetics of azithromycin following oral administration in older volunteers (65 to 85 years old) were similar to those in younger volunteers (18 to 40 years old) for the 5-day therapeutic regimen [see Geriatric Use 8.5)].
Drug Interactions Studies
Drug interaction studies were performed with oral azithromycin and other drugs likely to be co-administered. The effects of co-administration of azithromycin on the pharmacokinetics of other drugs are shown in Table 1 and the effects of other drugs on the pharmacokinetics of azithromycin are shown in Table 2.
Co-administration of azithromycin at therapeutic doses had a modest effect on the pharmacokinetics of the drugs listed in Table 1. No dosage adjustment of drugs listed in Table 1 is recommended when co-administered with azithromycin.
Co-administration of azithromycin with efavirenz or fluconazole had a modest effect on the pharmacokinetics of azithromycin. Nelfinavir significantly increased the C max and AUC of azithromycin. No dosage adjustment of azithromycin is recommended when administered with drugs listed in Table 2 [see Drug Interactions ( 7.3)].
Table 1. Drug Interactions: Pharmacokinetic Parameters for Co-administered Drugs in the Presence of Azithromycin * - 90% Confidence interval not reported
Co-administered
DrugDose of
Co-administered
DrugDose of
Azithromycinn Ratio (with/without azithromycin) of
Co-administered Drug Pharmacokinetic Parameters (90% CI); No Effect = 1Mean Cmax Mean AUC Atorvastatin 10 mg/day for 8 days 500 mg/day orally on days 6 to 8 12 0.83 (0.63 to 1.08) 1.01 (0.81 to 1.25) Carbamazepine 200 mg/day for 2 days, then 200 mg twice a day for 18 days
500 mg/day orally for days 16 to 18
7
0.97 (0.88 to 1.06)
0.96 (0.88 to 1.06)
Cetirizine
20 mg/day for 11 days500 mg orally on day 7, then 250 mg/day on days 8 to 11
14
1.03 (0.93 to 1.14)
1.02 (0.92 to 1.13)Didanosine
200 mg orally twice a day for 21 days1,200 mg/day orally on days 8 to 21
6
1.44 (0.85 to 2.43)
1.14 (0.83 to 1.57)Efavirenz
400 mg/day for 7 days600 mg orally on day 7
14
1.04*
0.95*Fluconazole 200 mg orally single dose 1,200 mg orally single dose
181.04 (0.98 to 1.11) 1.01 (0.97 to 1.05) Indinavir 800 mg three times a day for 5 days 1,200 mg orally on day 5
180.96 (0.86 to 1.08) 0.90 (0.81 to 1.00) Midazolam 15 mg orally on day 3 500 mg/day orally for 3 days
121.27 (0.89 to 1.81) 1.26 (1.01 to 1.56) Nelfinavir 750 mg three times a day for 11 days 1,200 mg orally on day 9
140.90 (0.81 to 1.01) 0.85 (0.78 to 0.93) Sildenafil 100 mg on days 1 and 4 500 mg/day orally for 3 days
121.16 (0.86 to 1.57) 0.92 (0.75 to 1.12)
Theophylline4 mg/kg IV on days 1, 11, 25 500 mg orally on day 7, 250 mg/day on days 8 to 11 10 1.19 (1.02 to 1.40) 1.02 (0.86 to 1.22)
Theophylline300 mg orally BID ×15 days 500 mg orally on day 6, then 250 mg/day on days
7 to 108 1.09 (0.92 to 1.29) 1.08 (0.89 to 1.31)
Triazolam0.125 mg on day 2 500 mg orally on day 1, then 250 mg/day on day 2 12 1.06* 1.02*
Trimethoprim/ Sulfamethoxazole160 mg/800 mg/day orally for 7 days 1,200 mg orally on day 7 12 0.85 (0.75 to 0.97)/ 0.90 (0.78 to 1.03) 0.87 (0.80 to 0.95/ 0.96 (0.88 to 1.03)
Zidovudine500 mg/day orally for 21 days 600 mg/day orally for 14 days
51.12 (0.42 to 3.02) 0.94 (0.52 to 1.70)
Zidovudine500 mg/day orally for 21 days 1,200 mg/day orally for 14 days
41.31 (0.43 to 3.97) 1.30 (0.69 to 2.43) Table 2. Drug Interactions: Pharmacokinetic Parameters for Azithromycin in the Presence of Co-administered Drugs [see Drug Interactions ( 7.3)]. * - 90% Confidence interval not reported
Co-administered
DrugDose of
Co-administered
DrugDose of
Azithromycinn Ratio (with/without co-administered drug) of Azithromycin Pharmacokinetic Parameters (90% CI); No Effect = 1 Mean
CmaxMean
AUCEfavirenz 400 mg/day for 7 days
600 mg orally on day 7
141.22
(1.04 to 1.42)
0.92*Fluconazole 200 mg orally single dose 1,200 mg orally single dose
180.82
(0.66 to 1.02)
1.07
(0.94 to 1.22)Nelfinavir 750 mg three times a day for 11 days 1,200 mg orally on day 9
142.36
(1.77 to 3.15)
2.12
(1.80 to 2.50)12.4 Microbiology
Mechanism of Action
Azithromycin acts by binding to the 23S rRNA of the 50S ribosomal subunit of susceptible microorganisms inhibiting bacterial protein synthesis and impeding the assembly of the 50S ribosomal subunit.
Resistance
Azithromycin demonstrates cross-resistance with erythromycin. The most frequently encountered mechanism of resistance to azithromycin is modification of the 23S rRNA target, most often by methylation. Ribosomal modifications can determine cross resistance to other macrolides, lincosamides and streptogramin B (MLSB phenotype).
Antimicrobial Activity
Azithromycin has been shown to be active against the following microorganisms, both in vitro and in clinical infections [see Indications and Usage ( 1)].
Gram-positive Bacteria
Staphylococcus aureus
Streptococcus pneumoniaeGram-negative Bacteria
Haemophilus influenzae
Moraxella catarrhalis
Neisseria gonorrhoeae
Legionella pneumophilaOther Bacteria
Chlamydophila pneumoniae
Chlamydia trachomatis
Mycoplasma hominis
Mycoplasma pneumoniaeThe following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for azithromycin against isolates of similar genus or organism group. However, the efficacy of azithromycin in treating clinical infections caused by these bacteria have not been established in adequate and well-controlled clinical trials.
Aerobic Gram-Positive Bacteria
Streptococci (Groups C, F, G)
Viridans group streptococciGram-Negative Bacteria
Bordetella pertussisAnaerobic Bacteria
Peptostreptococcus species
Prevotella biviaOther Bacteria
Ureaplasma urealyticum -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed to evaluate carcinogenic potential. Azithromycin has shown no mutagenic potential in standard laboratory tests: mouse lymphoma assay, human lymphocyte clastogenic assay, and mouse bone marrow clastogenic assay. In fertility studies conducted in male and female rats, oral administration of azithromycin for 64 to 66 days (males) or 15 days (females) prior to and during cohabitation resulted in decreased pregnancy rate at 20 and 30 mg/kg/day when both males and females were treated with azithromycin. This minimal effect on pregnancy rate (approximately 12% reduction compared to concurrent controls) did not become more pronounced when the dose was increased from 20 to 30 mg/kg/day (approximately 0.4 to 0.6 times the adult daily dose of 500 mg based on body surface area) and it was not observed when only one animal in the mated pair was treated. There were no effects on any other reproductive parameters, and there were no effects on fertility at 10 mg/kg/day. The relevance of these findings to patients being treated with azithromycin at the doses and durations recommended in the prescribing information is uncertain.
13.2 Animal Toxicology and/or Pharmacology
Phospholipidosis (intracellular phospholipid accumulation) has been observed in some tissues of mice, rats, and dogs given multiple oral doses of azithromycin. It has been demonstrated in numerous organ systems (e.g., eye, dorsal root ganglia, liver, gallbladder, kidney, spleen, and/or pancreas) in dogs and rats treated with azithromycin at doses which, expressed on the basis of body surface area, are similar to or less than the highest recommended adult human dose. This effect has been shown to be reversible after cessation of azithromycin treatment. Based on the pharmacokinetic data, phospholipidosis has been seen in the rat (50 mg/kg/day dose) at the observed maximal plasma concentration of 1.3 mcg/mL (1.6 times the observed C max of 0.821 mcg/mL at the adult dose of 2 g). Similarly, it has been shown in the dog (10 mg/kg/day dose) at the observed maximal serum concentration of 1 mcg/mL (1.2 times the observed C max of 0.821 mcg/mL at the adult dose of 2 g).
Phospholipidosis was also observed in neonatal rats dosed for 18 days at 30 mg/kg/day, which is less than the pediatric dose of 60 mg/kg based on body surface area. It was not observed in neonatal rats treated for 10 days at 40 mg/kg/day with mean maximal serum concentrations of 1.86 mcg/mL, approximately 1.5 times the C max of 1.27 mcg/mL at the pediatric dose. Phospholipidosis has been observed in neonatal dogs (10 mg/kg/day) at maximum mean whole blood concentrations of 3.54 mcg/mL, approximately 3 times the pediatric dose C max. The significance of the findings for animals and for humans is unknown.
-
14 CLINICAL STUDIES
14.1 Community-Acquired Pneumonia
In a controlled trial of community-acquired pneumonia performed in the U.S., azithromycin (500 mg as a single daily dose by the intravenous route for 2 to 5 days, followed by 500 mg/day by the oral route to complete 7 to 10 days therapy) was compared to cefuroxime (2,250 mg/day in three divided doses by the intravenous route for 2 to 5 days followed by 1,000 mg/day in two divided doses by the oral route to complete 7 to 10 days therapy), with or without erythromycin. For the 291 patients who were evaluable for clinical efficacy, the clinical outcome rates, i.e., cure, improved, and success (cure + improved) among the 277 patients seen at 10 to 14 days post-therapy were as follows:
Clinical Outcome Azithromycin Comparator Cure 46% 44% Improved 32% 30% Success (Cure + Improved) 78% 74% In a separate, uncontrolled clinical and microbiological trial performed in the U.S., 94 patients with community-acquired pneumonia who received azithromycin in the same regimen were evaluable for clinical efficacy. The clinical outcome rates, i.e., cure, improved, and success (cure + improved) among the 84 patients seen at 10 to 14 days post-therapy were as follows:
Clinical Outcome Azithromycin Cure 60% Improved 29% Success (Cure + Improved) 89% Microbiological determinations in both trials were made at the pre-treatment visit and, where applicable, were reassessed at later visits. Serological testing was done on baseline and final visit specimens. The following combined presumptive bacteriological eradication rates were obtained from the evaluable groups:
Combined Bacteriological Eradication Rates for Azithromycin:
a Nineteen of twenty-four patients (79%) with positive blood cultures for S. pneumoniae were cured (intent-to-treat analysis) with eradication of the pathogen.
(at last completed visit) Azithromycin S. pneumoniae 64/67 (96%) a H. influenzae 41/43 (95%) M. catarrhalis 9/10 (90%) S. aureus 9/10 (90%) The presumed bacteriological outcomes at 10 to 14 days post-therapy for patients treated with azithromycin with evidence (serology and/or culture) of atypical pathogens for both trials were as follows:
Evidence of Infection Total Cure Improved Cure + Improved Mycoplasma pneumoniae 18 11 (61%) 5 (28%) 16 (89%) Chlamydia pneumoniae 34 15 (44%) 13 (38%) 28 (82%) Legionella pneumophila 16 5 (31%) 8 (50%) 13 (81%) -
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Azithromycin for injection, USP is supplied in lyophilized form under a vacuum in a
10 mL vial equivalent to 500 mg of azithromycin for intravenous administration. Each vial also contains sodium hydroxide and 413.6 mg citric acid.
Product Code Unit of Sale Strength Each PRX309810 NDC 63323-398-14
Unit of 10500 mg per vial NDC 63323-398-41
10 mL single-dose vialThis container closure is not made with natural rubber latex.
Storage
Store the white to off-white lyophilized cake at 20º to 25ºC (68º to 77ºF) [see USP Controlled Room Temperature]. When diluted according to the instructions (1 mg/mL to 2 mg/mL), azithromycin for injection, USP is stable for 24 hours at or below room temperature 30ºC (86ºF), or for 7 days if stored under refrigeration 5ºC (41ºF).
-
17 PATIENT COUNSELING INFORMATION
Patients should be informed of the following serious and potentially serious adverse reactions that have been associated with azithromycin for injection, USP.
Diarrhea: Inform patients that diarrhea is a common problem caused by antibacterial drugs which usually ends when the antibacterial is discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial. If this occurs, patients should notify their physician as soon as possible.
The brand names mentioned in this document are the trademarks of their respective owners.
PREMIERProRx ® is a registered trademark of Premier Healthcare Alliance, L.P., used under license.
Manufactured by:
Fresenius Kabi
Lake Zurich, IL 60047
www.fresenius-kabi.com/us
451399A
Revised: September 2019 - PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
AZITHROMYCIN
azithromycin monohydrate injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63323-398 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AZITHROMYCIN MONOHYDRATE (UNII: JTE4MNN1MD) (AZITHROMYCIN ANHYDROUS - UNII:J2KLZ20U1M) AZITHROMYCIN ANHYDROUS 500 mg in 5 mL Inactive Ingredients Ingredient Name Strength SODIUM HYDROXIDE (UNII: 55X04QC32I) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63323-398-14 10 in 1 TRAY 03/20/2006 1 NDC:63323-398-41 5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065179 03/20/2006 Labeler - Fresenius Kabi USA, LLC (608775388) Establishment Name Address ID/FEI Business Operations Fresenius Kabi USA, LLC 023648251 manufacture(63323-398)