Label: OTEZLA- apremilast tablet, film coated
OTEZLA- apremilast kit
-
NDC Code(s):
55513-137-60,
55513-137-95,
55513-369-55,
55513-485-95, view more55513-485-96, 55513-497-23, 55513-497-51, 55513-497-60, 55513-508-55, 55513-518-04, 55513-996-95, 55513-996-96
- Packager: Amgen Inc
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated May 1, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OTEZLA safely and effectively. See full prescribing information for OTEZLA.
OTEZLA® (apremilast) tablets, for oral use
Initial U.S. Approval: 2014RECENT MAJOR CHANGES
INDICATIONS AND USAGE
OTEZLA, an inhibitor of phosphodiesterase 4 (PDE4), is indicated for the treatment of:
- Adult patients with active psoriatic arthritis (1.1)
- Adult patients with plaque psoriasis who are candidates for phototherapy or systemic therapy (1.2)
- Pediatric patients 6 years of age and older and weighing at least 20 kg with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy (1.2)
- Adult patients with oral ulcers associated with Behçet's Disease (1.3)
DOSAGE AND ADMINISTRATION
To reduce the risk of gastrointestinal symptoms, titrate to recommended dosage as follows:
- Adults with Plaque Psoriasis, Psoriatic Arthritis, or Behçet's Disease
- Pediatric Patients 6 Years of Age and Older and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis
-
Dosage in Severe Renal Impairment:
- Adult Patients: For initial dosage titration, titrate using only morning schedule listed in Table 1 and skip afternoon doses. Recommended maintenance dosage is 30 mg once daily (2.2)
- Pediatric Patients 6 Years of Age and Older and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis: For initial dosage titration, titrate using only morning schedule for appropriate body weight category in Table 2 and skip afternoon doses (2.2)
DOSAGE FORMS AND STRENGTHS
Tablets: 10 mg, 20 mg, 30 mg (3)
CONTRAINDICATIONS
Known hypersensitivity to apremilast or to any of the excipients in the formulation (4)
WARNINGS AND PRECAUTIONS
- Hypersensitivity: Cases of angioedema and anaphylaxis have been reported during post marketing surveillance. Avoid the use of OTEZLA in patients with known hypersensitivity to apremilast or to any of the excipients in the formulation. If signs or symptoms of serious hypersensitivity reactions develop during treatment, discontinue OTEZLA and institute appropriate therapy (5.1).
- Diarrhea, Nausea, and Vomiting: Consider OTEZLA dose reduction or suspension if patients develop severe diarrhea, nausea, or vomiting (5.2)
- Depression: Advise patients, their caregivers, and families to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes and if such changes occur to contact their healthcare provider. Carefully weigh risks and benefits of treatment with OTEZLA in patients with a history of depression and/or suicidal thoughts or behavior (5.3)
- Weight Decrease: Monitor weight regularly. If unexplained or clinically significant weight loss occurs, evaluate weight loss and consider discontinuation of OTEZLA (5.4)
- Drug Interactions: Use with strong cytochrome P450 enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine, phenytoin) is not recommended because loss of efficacy may occur (5.5, 7.1)
ADVERSE REACTIONS
- Psoriatic Arthritis: The most common adverse reactions (≥ 5%) are diarrhea, nausea, and headache (6.1)
- Plaque Psoriasis: The most common adverse reactions (≥ 5%) are diarrhea, nausea, upper respiratory tract infection, and headache, including tension headache (6.1)
- Behçet's Disease: The most common adverse reactions (≥ 10%) are diarrhea, nausea, headache, and upper respiratory tract infection (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Amgen Inc. at 1-800-77-AMGEN (1-800-772-6436) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
Severe Renal Impairment: Increased systemic exposure of OTEZLA has been observed. For adults and for pediatric patients weighing 50 kg or more, reduce dosage to 30 mg once daily. For pediatric patients weighing 20 kg to less than 50 kg, reduce dosage to 20 mg once daily (2.2, 8.6).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 4/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Psoriatic Arthritis
1.2 Plaque Psoriasis
1.3 Oral Ulcers Associated with Behçet's Disease
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Psoriatic Arthritis, Plaque Psoriasis, and Behçet's Disease
2.2 Dosage Adjustment in Patients with Severe Renal Impairment
2.3 Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
5.2 Diarrhea, Nausea, and Vomiting
5.3 Depression
5.4 Weight Decrease
5.5 Drug Interactions
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Strong CYP450 Inducers
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Psoriatic Arthritis
14.2 Adult Moderate to Severe Plaque Psoriasis
14.3 Pediatric Moderate to Severe Plaque Psoriasis
14.4 Adult Mild to Moderate Plaque Psoriasis
14.5 Oral Ulcers Associated with Behçet's Disease
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Psoriatic Arthritis
OTEZLA is indicated for the treatment of adult patients with active psoriatic arthritis.
1.2 Plaque Psoriasis
OTEZLA is indicated for the treatment of:
- Adult patients with plaque psoriasis who are candidates for phototherapy or systemic therapy.
- Pediatric patients 6 years of age and older and weighing at least 20 kg with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Psoriatic Arthritis, Plaque Psoriasis, and Behçet's Disease
Adult Patients with Psoriatic Arthritis, Plaque Psoriasis, or Behçet's Disease
The recommended initial dosage titration of OTEZLA from Day 1 to Day 5 is shown in Table 1. Following the 5-day titration, the recommended maintenance dosage is 30 mg twice daily taken orally starting on Day 6. This titration is intended to reduce the gastrointestinal symptoms associated with initial therapy.
Table 1: Dosage Titration Schedule for Adult Patients with Psoriatic Arthritis, Plaque Psoriasis, or Behçet's Disease Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 & thereafter AM AM PM AM PM AM PM AM PM AM PM 10 mg 10 mg 10 mg 10 mg 20 mg 20 mg 20 mg 20 mg 30 mg 30 mg 30 mg Pediatric Patients 6 Years of Age and Older and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis
The recommended dosage for pediatric patients 6 years of age and older and weighing at least 20 kg with moderate to severe plaque psoriasis is based on body weight. Following the appropriate initial titration schedule shown in Table 2, the recommended maintenance dosage of OTEZLA taken orally is 30 mg twice daily for pediatric patients who weigh at least 50 kg and 20 mg twice daily for pediatric patients who weigh from 20 kg to less than 50 kg. This titration is intended to reduce the gastrointestinal symptoms associated with initial therapy.
Table 2: Dosage Titration Schedule for Pediatric Patients 6 Years of Age and Older and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis Body Weight Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 & thereafter AM AM PM AM PM AM PM AM PM AM PM 50 kg or more 10 mg 10 mg 10 mg 10 mg 20 mg 20 mg 20 mg 20 mg 30 mg 30 mg 30 mg 20 kg to less than 50 kg 10 mg 10 mg 10 mg 10 mg 20 mg 20 mg 20 mg 20 mg 20 mg 20 mg 20 mg 2.2 Dosage Adjustment in Patients with Severe Renal Impairment
Adult Patients with Psoriatic Arthritis, Plaque Psoriasis, or Behçet's Disease
For initial dosage titration in adult patients with severe renal impairment (creatinine clearance [CLcr] of less than 30 mL per minute estimated by the Cockcroft–Gault equation), titrate OTEZLA using only the AM schedule listed in Table 1 and skip the PM doses. Reduce OTEZLA maintenance dosage to 30 mg once daily in this group [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
Pediatric Patients 6 Years of Age and Older and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis
For initial dosage titration in pediatric patients 6 years of age and older and weighing at least 20 kg with moderate to severe plaque psoriasis and severe renal impairment (CLcr of less than 30 mL per minute estimated by the Cockcroft–Gault equation), titrate OTEZLA using only the AM schedule listed in Table 2 for the appropriate body weight category and skip the PM doses. Reduce the OTEZLA maintenance dosage to 30 mg once daily for pediatric patients who weigh at least 50 kg and to 20 mg once daily for pediatric patients who weigh 20 kg to less than 50 kg [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
-
3 DOSAGE FORMS AND STRENGTHS
OTEZLA is available as diamond shaped, film coated tablets in the following dosage strengths:
- 10-mg pink tablet engraved with "APR" on one side and "10" on the other side
- 20-mg brown tablet engraved with "APR" on one side and "20" on the other side
- 30-mg beige tablet engraved with "APR" on one side and "30" on the other side
-
4 CONTRAINDICATIONS
OTEZLA is contraindicated in patients with a known hypersensitivity to apremilast or to any of the excipients in the formulation [see Adverse Reactions (6.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
Hypersensitivity reactions, including cases of angioedema and anaphylaxis, have been reported during post marketing surveillance. Avoid the use of OTEZLA in patients with known hypersensitivity to apremilast or to any of the excipients in the formulation. If signs or symptoms of serious hypersensitivity reactions develop during treatment, discontinue OTEZLA and institute appropriate therapy.
5.2 Diarrhea, Nausea, and Vomiting
There have been reports of severe diarrhea, nausea, and vomiting associated with the use of OTEZLA. Most events occurred within the first few weeks of treatment. In some cases, patients were hospitalized. Patients 65 years of age or older and patients taking medications that can lead to volume depletion or hypotension may be at a higher risk of complications from severe diarrhea, nausea, or vomiting. Monitor patients who are more susceptible to complications of diarrhea or vomiting. Patients who reduced dosage or discontinued OTEZLA generally improved quickly. Consider OTEZLA dose reduction or suspension if patients develop severe diarrhea, nausea, or vomiting.
5.3 Depression
Treatment with OTEZLA is associated with an increased incidence of depression. Before using OTEZLA in patients with a history of depression and/or suicidal thoughts or behavior, carefully weigh the risks and benefits of treatment with OTEZLA. Advise patients, their caregivers, and families of the need to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes, and if such changes occur to contact their healthcare provider. Carefully evaluate the risks and benefits of continuing treatment with OTEZLA if such events occur.
Psoriatic Arthritis: During the 16-week placebo-controlled period of the 3 controlled clinical trials, 1.0% (10/998) of subjects treated with OTEZLA reported depression or depressed mood compared to 0.8% (4/495) treated with placebo. During the clinical trials, 0.3% (4/1441) of subjects treated with OTEZLA discontinued treatment due to depression or depressed mood compared with none in placebo treated subjects (0/495). Depression was reported as serious in 0.2% (3/1441) of subjects exposed to OTEZLA, compared to none in placebo-treated subjects (0/495). Instances of suicidal ideation and behavior have been observed in 0.2% (3/1441) of subjects while receiving OTEZLA, compared to none in placebo treated subjects (0/495). In the clinical trials, 2 subjects who received placebo committed suicide compared to none in OTEZLA-treated subjects.
Plaque Psoriasis: During the 16-week placebo-controlled period of the 3 controlled clinical trials in adult subjects with moderate to severe plaque psoriasis, 1.3% (12/920) of subjects treated with OTEZLA reported depression compared to 0.4% (2/506) treated with placebo. During the clinical trials, 0.1% (1/1308) of subjects treated with OTEZLA discontinued treatment due to depression compared with none in placebo-treated subjects (0/506). Depression was reported as serious in 0.1% (1/1308) of subjects exposed to OTEZLA, compared to none in placebo-treated subjects (0/506). Instances of suicidal behavior have been observed in 0.1% (1/1308) of subjects while receiving OTEZLA, compared to 0.2% (1/506) in placebo-treated subjects. In the clinical trials, one subject treated with OTEZLA attempted suicide while one who received placebo committed suicide.
During the 16-week placebo-controlled period of the clinical trial in adults with mild to moderate plaque psoriasis, the incidence of subjects reporting depression was similar to what was observed in the adult moderate to severe plaque psoriasis trials.
Behçet's Disease: During the placebo-controlled period of the phase 3 trial, 1% (1/104) of subjects treated with OTEZLA reported depression/depressed mood compared to 1% (1/103) treated with placebo. None of these reports of depression was serious or led to discontinuation from the trial. No instances of suicidal ideation or behavior were reported during the placebo-controlled period of the phase 3 trial in subjects treated with OTEZLA (0/104) or treated with placebo (0/103).
5.4 Weight Decrease
Weight loss may occur in adult or pediatric patients treated with OTEZLA.
Regularly monitor the weight of patients treated with OTEZLA. If unexplained or clinically significant weight loss occurs, evaluate weight loss and consider discontinuation of OTEZLA [see Adverse Reactions (6.1)].
Weight Loss in Adult Patients
During the placebo-controlled period of the trials in psoriatic arthritis (PsA), weight decrease between 5%-10% of body weight was reported in 10% (49/497) of subjects treated with OTEZLA 30 mg twice daily compared to 3.3% (16/495) treated with placebo.
During the placebo-controlled period of the trials in adults with moderate to severe plaque psoriasis, weight decrease between 5%-10% of body weight occurred in 12% (96/784) of subjects treated with OTEZLA compared to 5% (19/382) treated with placebo. Weight decrease of ≥ 10% of body weight occurred in 2% (16/784) of subjects treated with OTEZLA 30 mg twice daily compared to 1% (3/382) subjects treated with placebo.
During the placebo-controlled period of the clinical trial in adults with mild to moderate plaque psoriasis, weight decrease was similar to what was observed in the trials of adults with moderate to severe plaque psoriasis.
During the placebo-controlled period of the phase 3 trial in Behçet's Disease, weight decrease > 5% of body weight was reported in 4.9% (5/103) of subjects treated with OTEZLA 30 mg twice daily compared to 3.9% (4/102) subjects treated with placebo.
Weight Loss in Pediatric Patients
During the placebo-controlled period of the clinical trial in pediatric subjects 6 to 17 years of age with moderate to severe plaque psoriasis, weight decrease between 5%-10% of body weight occurred in 12% (19/163) of pediatric subjects treated with OTEZLA compared to 2.5% (2/80) of pediatric subjects treated with placebo. Weight decrease of ≥ 10% of body weight occurred in 1% (1/163) of pediatric subjects treated with OTEZLA twice daily compared to 0% (0/80) of pediatric subjects treated with placebo.
Closely monitor growth (height and weight) in OTEZLA-treated pediatric patients. Pediatric patients who are not growing or gaining weight as expected may need to have their treatment interrupted.
5.5 Drug Interactions
Co-administration of strong cytochrome P450 enzyme inducer, rifampin, resulted in a reduction of systemic exposure of apremilast, which may result in a loss of efficacy of OTEZLA. Therefore, the use of cytochrome P450 enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine, phenytoin) with OTEZLA is not recommended [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
-
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in the labeling:
- Hypersensitivity [see Warnings and Precautions (5.1)]
- Diarrhea, Nausea, and Vomiting [see Warnings and Precautions (5.2)]
- Depression [see Warnings and Precautions (5.3)]
- Weight Decrease [see Warnings and Precautions (5.4)]
- Drug Interactions [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Psoriatic Arthritis Clinical Trials
OTEZLA was evaluated in 3 multicenter, randomized, double-blind, placebo-controlled trials (PsA-1, PsA-2, and PsA-3) of similar design in adult subjects with active psoriatic arthritis [see Clinical Studies (14.1)]. Across the 3 trials, there were 1493 subjects randomized equally to placebo, OTEZLA 20 mg twice daily or OTEZLA 30 mg twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Placebo subjects whose tender and swollen joint counts had not improved by at least 20% were re-randomized 1:1 in a blinded fashion to either OTEZLA 20 mg twice daily or 30 mg twice daily at week 16 while OTEZLA subjects remained on their initial treatment. Subjects ranged in age from 18 to 83 years, with an overall median age of 51 years.
The majority of the most common adverse reactions presented in Table 3 occurred within the first 2 weeks of treatment and tended to resolve over time with continued dosing. Diarrhea, headache, and nausea were the most commonly reported adverse reactions. The most common adverse reactions leading to discontinuation for subjects taking OTEZLA were nausea (1.8%), diarrhea (1.8%), and headache (1.2%). The proportion of subjects with psoriatic arthritis who discontinued treatment due to any adverse reaction was 4.6% for subjects taking OTEZLA 30 mg twice daily and 1.2% for placebo-treated subjects.
Table 3: Adverse Reactions Reported in ≥ 2% of Adult Subjects with Active Psoriatic Arthritis on OTEZLA 30 mg Twice Daily and ≥ 1% than That Observed in Subjects on Placebo up to Day 112 (Week 16) Placebo OTEZLA 30 mg BID* Adverse Reactions Day 1 to 5
(N = 495)
n (%)†Day 6 to Day 112
(N = 490)
n (%)Day 1 to 5
(N = 497)
n (%)Day 6 to Day 112
(N = 493)
n (%)- *
- BID = twice daily.
- †
- n (%) indicates number of subjects and percent.
- ‡
- Of the reported gastrointestinal adverse reactions, 1 subject experienced a serious adverse reaction of nausea and vomiting in OTEZLA 30 mg twice daily; 1 subject treated with OTEZLA 20 mg twice daily experienced a serious adverse reaction of diarrhea; 1 subject treated with OTEZLA 30 mg twice daily experienced a serious adverse reaction of headache.
- §
- Of the reported adverse drug reactions none were serious.
Diarrhea‡ 6 (1.2) 8 (1.6) 46 (9.3) 38 (7.7) Nausea‡ 7 (1.4) 15 (3.1) 37 (7.4) 44 (8.9) Headache‡ 9 (1.8) 11 (2.2) 24 (4.8) 29 (5.9) Upper respiratory tract infection§ 3 (0.6) 9 (1.8) 3 (0.6) 19 (3.9) Vomiting‡ 2 (0.4) 2 (0.4) 4 (0.8) 16 (3.2) Nasopharyngitis§ 1 (0.2) 8 (1.6) 1 (0.2) 13 (2.6) Abdominal pain upper§ 0 (0.0) 1 (0.2) 3 (0.6) 10 (2.0) Moderate to Severe Plaque Psoriasis Clinical Trials
Adverse Reactions from Clinical Trials in Adults
The safety of OTEZLA was assessed in 1426 subjects in 3 randomized, double-blind, placebo-controlled trials in adult subjects with moderate to severe plaque psoriasis who were candidates for phototherapy or systemic therapy. Subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Subjects ranged in age from 18 to 83 years, with an overall median age of 46 years.
Diarrhea, nausea, and upper respiratory tract infection were the most commonly reported adverse reactions (see Table 4). The most common adverse reactions leading to discontinuation for subjects taking OTEZLA were nausea (1.6%), diarrhea (1.0%), and headache (0.8%). The proportion of subjects with plaque psoriasis who discontinued treatment due to any adverse reaction was 6.1% for subjects treated with OTEZLA 30 mg twice daily and 4.1% for placebo-treated subjects.
Table 4: Adverse Reactions Reported in ≥ 1% of Adult Subjects with Moderate to Severe Plaque Psoriasis on OTEZLA and With Greater Frequency Than in Subjects on Placebo up to Day 112 (Week 16) Adverse Reactions Placebo (N = 506)
n (%)OTEZLA 30 mg BID* (N = 920)
n (%)Diarrhea 32 (6) 160 (17) Nausea 35 (7) 155 (17) Upper respiratory tract infection 31 (6) 84 (9) Tension headache 21 (4) 75 (8) Headache 19 (4) 55 (6) Abdominal pain† 11 (2) 39 (4) Vomiting 8 (2) 35 (4) Fatigue 9 (2) 29 (3) Dyspepsia 6 (1) 29 (3) Decreased appetite 5 (1) 26 (3) Insomnia 4 (1) 21 (2) Back pain 4 (1) 20 (2) Migraine 5 (1) 19 (2) Frequent bowel movements 1 (0) 17 (2) Depression 2 (0) 12 (1) Bronchitis 2 (0) 12 (1) Tooth abscess 0 (0) 10 (1) Folliculitis 0 (0) 9 (1) Sinus headache 0 (0) 9 (1) Severe worsening of psoriasis (rebound) occurred in 0.3% (4/1184) subjects following discontinuation of treatment with OTEZLA.
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (PSOR-3) in adults with moderate to severe plaque psoriasis of the scalp [see Clinical Studies (14.2)]. A total of 302 subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. The most commonly reported adverse reactions that occurred at a higher rate in the OTEZLA group than in the placebo group were: diarrhea (31% vs. 11%), nausea (22% vs. 6%), headache (12% vs. 5%), and vomiting (6% vs. 2%). The proportion of subjects who discontinued treatment because of any adverse reaction during the 16-week placebo-controlled period of the trial was 6% for subjects who received OTEZLA 30 mg twice daily and 3% for subjects who received placebo. Gastrointestinal adverse reactions that led to discontinuation of treatment were diarrhea (3% vs. 0%), nausea (1.5% vs. 1%), and vomiting (1.5% vs. 0 %) in the OTEZLA group compared to placebo.
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (PSOR-5) in adults with moderate to severe plaque psoriasis of the genital area [see Clinical Studies (14.2)]. A total of 289 subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. Overall, the safety profile observed in the OTEZLA group during the placebo-controlled phase was consistent with the safety profile previously established in adult subjects with moderate to severe plaque psoriasis.
Adverse Reactions from Clinical Trials in Pediatric Subjects 6 to 17 Years of Age
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (PSOR-6) in pediatric subjects 6 to 17 years of age with moderate to severe plaque psoriasis [see Clinical Studies (14.3)]. A total of 245 subjects were randomized to receive OTEZLA (163 subjects, at a dosage of 20 mg twice daily or 30 mg twice daily, based on body weight) or placebo (82 subjects) twice daily during the 16-week placebo-controlled phase of the trial. The trial also included a 36-week extension phase during which all subjects received OTEZLA 20 mg or 30 mg twice daily. Overall, the safety profile observed in pediatric subjects treated with OTEZLA during the study was consistent with the safety profile established in adult subjects with moderate to severe plaque psoriasis.
Mild to Moderate Plaque Psoriasis Clinical Trial in Adults
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (PSOR-4) in adult subjects with mild to moderate plaque psoriasis [see Clinical Studies (14.3)]. A total of 595 subjects were randomized to receive OTEZLA 30 mg twice daily (297 subjects) or placebo twice daily (298 subjects) during the placebo-controlled phase of the trial. The trial also included an open label extension phase during which all subjects received OTEZLA 30 mg twice daily. Overall, the safety profile observed in the OTEZLA group during the placebo-controlled phase was consistent with the safety profile previously established in adult subjects with moderate to severe plaque psoriasis.
Behçet's Disease Clinical Trials
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (BCT-002) in adult subjects with Behçet's Disease (BD) with active oral ulcers [see Clinical Studies (14.4)]. A total of 207 subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. After Week 12, all subjects received treatment with OTEZLA 30 mg twice daily. Subjects ranged in age from 19 to 72, with a mean age of 40 years.
Diarrhea, nausea, headache, and upper respiratory tract infection were the most commonly reported adverse reactions (see Table 5). The proportion of subjects with BD who discontinued treatment due to any adverse reaction during the placebo-controlled period of the trial, was 2.9% for subjects treated with OTEZLA 30 mg twice daily and 4.9% for placebo-treated subjects.
Table 5: Adverse Reactions Reported in ≥ 5% of Adult Subjects with BD with Active Oral Ulcers on OTEZLA and with at Least 1% Greater Frequency than Subjects on Placebo up to Week 12 Adverse Reactions Placebo
(N = 103)
n (%)OTEZLA 30 mg twice daily
(N = 104)
n (%)- *
- There were no serious adverse reactions of diarrhea, nausea or vomiting.
Diarrhea* 21 (20.4) 43 (41.3) Nausea* 11 (10.7) 20 (19.2) Headache 11 (10.7) 15 (14.4) Upper respiratory tract infection 5 (4.9) 12 (11.5) Abdominal pain upper 2 (1.9) 9 (8.7) Vomiting* 2 (1.9) 9 (8.7) Back pain 6 (5.8) 8 (7.7) Viral upper respiratory tract infection 5 (4.9) 7 (6.7) Arthralgia 3 (2.9) 6 (5.8) Other adverse reactions reported in subjects on OTEZLA in psoriatic arthritis, plaque psoriasis, and Behçet's Disease clinical trials are:
- Gastrointestinal Disorders: Gastroesophageal reflux disease
- Immune System Disorders: Hypersensitivity
- Investigations: Weight decrease
- Metabolism and Nutrition Disorders: Decreased appetite1
- Nervous System Disorders: Migraine
- Respiratory, Thoracic, and Mediastinal Disorders: Cough
- Skin and Subcutaneous Tissue Disorders: Rash
- 1
- 1 subject treated with OTEZLA 30 mg twice daily experienced a serious adverse reaction.
-
7 DRUG INTERACTIONS
7.1 Strong CYP450 Inducers
Apremilast exposure is decreased when OTEZLA is co-administered with strong CYP450 inducers (such as rifampin) and may result in loss of efficacy [see Warnings and Precautions (5.5) and Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to OTEZLA during pregnancy. Information about the registry can be obtained by calling 1-877-311-8972 or visiting https://mothertobaby.org/ongoing-study/otezla/.
Risk Summary
Available pharmacovigilance data with OTEZLA use in pregnant women have not established a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes, but these data are extremely limited. Based on findings from animal reproduction studies, OTEZLA may increase the risk for fetal loss. In animal embryo-fetal development studies, the administration of apremilast to pregnant cynomolgus monkeys during organogenesis resulted in dose-related increases in abortion/embryo-fetal death at dose exposures 2.1-times the maximum recommended human therapeutic dose (MRHD) and no adverse effect at an exposure of 1.4-times the MRHD. When administered to pregnant mice, during organogenesis there were no apremilast-induced malformations up to exposures 4.0-times the MRHD (see Data). Advise pregnant women of the potential risk of fetal loss. Consider pregnancy planning and prevention for females of reproductive potential.
The background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Animal Data
In an embryo-fetal developmental study, pregnant cynomolgus monkeys were administered apremilast at doses of 20, 50, 200, or 1000 mg/kg/day during the period of organogenesis (gestation Days 20 through 50). There was a dose-related increase in spontaneous abortions, with most abortions occurring during Weeks 3 to 4 of dosing in the first trimester, at doses approximately 2.1-times the MRHD and greater (on an area under the curve [AUC] basis at doses ≥ 50 mg/kg/day). No abortifacient effects were observed at a dose approximately 1.4-times the MRHD (on an AUC basis at a dose of 20 mg/kg/day). Although, there was no evidence for a teratogenic effect at doses of 20 mg/kg/day and greater when examined at Day 100, aborted fetuses were not examined.
In an embryo-fetal development study in mice, apremilast was administered at doses of 250, 500, or 750 mg/kg/day to dams during organogenesis (gestation Day 6 through 15). In a combined fertility and embryo-fetal development study in mice, apremilast was administered at doses of 10, 20, 40, or 80 mg/kg/day starting 15 days before cohabitation and continuing through gestation Day 15. No teratogenic findings attributed to apremilast were observed in either study; however, there was an increase in post-implantation loss at doses corresponding to a systemic exposure of 2.3-times the MRHD and greater (≥ 20 mg/kg/day). At doses of ≥ 20 mg/kg/day skeletal variations included incomplete ossification sites of tarsals, skull, sternebra, and vertebrae. No effects were observed at a dose approximately 1.3-times the MRHD (10 mg/kg/day).
Apremilast distributed across the placenta into the fetal compartment in mice and monkeys.
In a pre and postnatal study in mice, apremilast was administered to pregnant female mice at doses of 10, 80, or 300 mg/kg/day from Day 6 of gestation through Day 20 of lactation, with weaning on Day 21. Dystocia, reduced viability, and reduced birth weights occurred at doses corresponding to ≥ 4.0-times the MRHD (on an AUC basis at doses ≥ 80 mg/kg/day). No adverse effects occurred at a dose 1.3-times the MRHD (10 mg/kg/day). There was no evidence for functional impairment of physical development, behavior, learning ability, immune competence, or fertility in the offspring at doses up to 7.5-times the MRHD (on an AUC basis at a dose of 300 mg/kg/day).
8.2 Lactation
Risk Summary
There are no data on the presence of apremilast in human milk, the effects on the breastfed infant, or the effects on milk production. However, apremilast was detected in the milk of lactating mice. When a drug is present in animal milk, it is likely that the drug will be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for OTEZLA and any potential adverse effects on the breastfed infant from OTEZLA or from the underlying maternal condition.
8.4 Pediatric Use
Plaque Psoriasis
The safety and effectiveness of OTEZLA have been established in pediatric patients 6 years of age and older and weighing at least 20 kg with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy. Use of OTEZLA in these patients is supported by evidence from a 52-week adequate and well-controlled clinical trial (PSOR-6) in 245 pediatric subjects 6 to 17 years of age with moderate to severe plaque psoriasis. Weight loss in OTEZLA-treated pediatric subjects was comparable to weight loss observed in adults. [see Warnings and Precautions (5.4), Adverse Reactions (6.1) and Clinical Studies (14.3)].
Closely monitor growth (height and weight) in OTEZLA-treated pediatric patients. Pediatric patients who are not growing or gaining weight as expected may need to have their treatment interrupted.
The safety and effectiveness of OTEZLA have not been established in pediatric patients below the age of 6 years or weighing less than 20 kg with moderate to severe plaque psoriasis.
8.5 Geriatric Use
Of the 1493 patients who enrolled in Trials PsA-1, PsA-2, and PsA-3, a total of 146 psoriatic arthritis patients were 65 years of age and older, including 19 patients 75 years and older. No overall differences were observed in the safety profile of geriatric patients ≥ 65 years of age and younger adult patients < 65 years of age in the clinical trials.
Of the 1257 subjects who enrolled in two placebo-controlled plaque psoriasis trials (PSOR-1 and PSOR-2), a total of 108 plaque psoriasis patients were 65 years of age and older, including 9 patients who were 75 years of age and older. No overall differences were observed in the safety or effectiveness in geriatric patients ≥ 65 years of age and younger adult patients < 65 years of age in the clinical trials.
Because patients 65 years of age or older may be at a higher risk of complications such as volume depletion or hypotension from severe diarrhea, nausea, or vomiting, monitor geriatric patients closely for such complications [see Warning and Precautions (5.2)].
8.6 Renal Impairment
Apremilast pharmacokinetics were characterized in adult subjects with mild, moderate, and severe renal impairment as defined by a creatinine clearance of 60-89, 30-59, and less than 30 mL per minute, respectively, by the Cockcroft–Gault equation. No dosage adjustment is needed in patients with mild or moderate renal impairment. In adult patients with severe renal impairment, reduce the maintenance dosage of OTEZLA to 30 mg once daily. In pediatric patients 6 years of age and older and weighing at least 20 kg with moderate to severe plaque psoriasis and severe renal impairment, reduce the maintenance dosage of OTEZLA to 30 mg once daily for pediatric patients weighing at least 50 kg and to 20 mg once daily for pediatric patients weighing 20 kg to less than 50 kg [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
The active ingredient in OTEZLA tablets is apremilast. Apremilast is a phosphodiesterase 4 (PDE4) inhibitor. Apremilast is known chemically as
N-[2-[(1S)-1-(3-ethoxy-4-methoxyphenyl)-2-(methylsulfonyl)ethyl]-2,3-dihydro-1,3-dioxo-1H-isoindol-4-yl]acetamide. Its empirical formula is C22H24N2O7S and the molecular weight is 460.5.The chemical structure is:
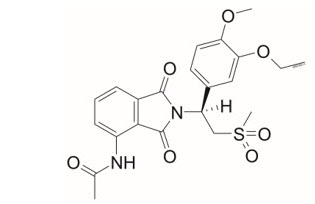
OTEZLA tablets are supplied in 10-, 20-, and 30-mg strengths for oral administration. Each tablet contains apremilast as the active ingredient and the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, croscarmellose sodium, magnesium stearate, polyvinyl alcohol, titanium dioxide, polyethylene glycol, talc, iron oxide red, iron oxide yellow (20 and 30 mg only) and iron oxide black (30 mg only).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Apremilast is an oral small molecule inhibitor of phosphodiesterase 4 (PDE4) specific for cyclic adenosine monophosphate (cAMP). PDE4 inhibition results in increased intracellular cAMP levels. The specific mechanism(s) by which apremilast exerts its therapeutic action is not well defined.
12.3 Pharmacokinetics
Absorption
Apremilast when taken orally is absorbed with an absolute bioavailability of ~73%, with peak plasma concentrations (Cmax) occurring at a median time (tmax) of ~2.5 hours. Co-administration with food does not alter the extent of absorption of apremilast.
Distribution
Human plasma protein binding of apremilast is approximately 68%. Mean apparent volume of distribution (Vd) is 87 L.
Metabolism
Following oral administration in humans, apremilast is a major circulating component (45%) followed by inactive metabolite M12 (39%), a glucuronide conjugate of O-demethylated apremilast. It is extensively metabolized in humans with up to 23 metabolites identified in plasma, urine and feces. Apremilast is metabolized by both cytochrome (CYP) oxidative metabolism with subsequent glucuronidation and non-CYP mediated hydrolysis. In vitro, CYP metabolism of apremilast is primarily mediated by CYP3A4, with minor contributions from CYP1A2 and CYP2A6.
Elimination
The plasma clearance of apremilast is about 10 L/hr in healthy subjects, with a terminal elimination half-life of approximately 6-9 hours. Following oral administration of radiolabeled apremilast, about 58% and 39% of the radioactivity is recovered in urine and feces, respectively, with about 3% and 7% of the radioactive dose recovered as apremilast in urine and feces, respectively.
Specific Populations
Patients with Hepatic Impairment: The pharmacokinetics of apremilast is not affected by moderate or severe hepatic impairment.
Patients with Renal Impairment: The pharmacokinetics of apremilast is not affected by mild or moderate renal impairment. In 8 adult subjects with severe renal impairment administered a single dose of 30 mg apremilast, the AUC and Cmax of apremilast increased by approximately 88% and 42%, respectively [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
Geriatric Patients: A single oral dose of 30-mg apremilast was studied in young adults and elderly healthy subjects. The apremilast exposure in elderly subjects (65 to 85 years of age) was about 13% higher in AUC and about 6% higher in Cmax than in young subjects (18 to 55 years of age) [see Use in Specific Populations (8.5)].
Pediatric Patients: The pharmacokinetics of OTEZLA were evaluated in a clinical trial in pediatric subjects 6 to 17 years of age with moderate to severe plaque psoriasis at the recommended pediatric dosage regimen [see Dosage and Administration (2.1) and Clinical Studies (14.3)]. Population pharmacokinetic analysis indicated that steady-state exposure (AUC and Cmax) of OTEZLA in pediatric subjects receiving the pediatric maintenance dosage regimen (20 or 30 mg twice daily, based on body weight) was comparable to steady-state exposure in adult subjects at the 30 mg twice daily dosage.
Male and Female Patients: In pharmacokinetic trials in healthy volunteers, the extent of exposure in females was about 31% higher and Cmax was about 8% higher than that in male subjects.
Racial or Ethnic Groups: The pharmacokinetics of apremilast in Chinese and Japanese healthy male subjects is comparable to that in White healthy male subjects. In addition, apremilast exposure is similar among White subjects (including Hispanic or Latino and not Hispanic or Latino subjects) and Black or African American subjects.
Drug Interactions
In vitro data: Apremilast is not an inhibitor of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, or CYP3A4 and not an inducer of CYP1A2, CYP2B6, CYP2C9, CYP2C19, or CYP3A4. Apremilast is a substrate, but not an inhibitor of P-glycoprotein (P-gp) and is not a substrate or an inhibitor of organic anion transporter (OAT)1 and OAT3, organic cation transporter (OCT)2, organic anion transporting polypeptide (OATP)1B1 and OATP1B3, or breast cancer resistance protein (BCRP).
Drug interaction trials were performed with apremilast and CYP3A4 substrates (oral contraceptive containing ethinyl estradiol and norgestimate), CYP3A and P-gp inhibitor (ketoconazole), CYP450 inducer (rifampin) and frequently co-administered drug in this patient population (methotrexate).
No significant pharmacokinetic interactions were observed when 30-mg oral apremilast was administered with either oral contraceptive, ketoconazole, or methotrexate. Co-administration of the CYP450 inducer rifampin (600 mg once daily for 15 days) with a single oral dose of 30-mg apremilast resulted in reduction of apremilast AUC and Cmax by 72% and 43%, respectively [see Warnings and Precautions (5.5) and Drug Interactions (7.1)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies were conducted in mice and rats with apremilast to evaluate its carcinogenic potential. No evidence of apremilast-induced tumors was observed in mice at oral doses up to 8.8-times the Maximum Recommended Human Dose (MRHD) on an AUC basis (1000 mg/kg/day) or in rats at oral doses up to approximately 0.08- and 1.1-times the MRHD, (20 mg/kg/day in males and 3 mg/kg/day in females, respectively).
Apremilast tested negative in the Ames assay, in vitro chromosome aberration assay of human peripheral blood lymphocytes, and the in vivo mouse micronucleus assay.
In a fertility study of male mice, apremilast at oral doses up to approximately 3-times the MRHD based on AUC (up to 50 mg/kg/day) produced no effects on male fertility. In a fertility study of female mice, apremilast was administered at oral doses of 10, 20, 40, or 80 mg/kg/day. At doses ≥ 1.8-times the MRHD (≥ 20 mg/kg/day), estrous cycles were prolonged, due to lengthening of diestrus which resulted in a longer interval until mating. Mice that became pregnant at doses of 20 mg/kg/day and greater also had increased incidences of early post-implantation losses. There was no effect of apremilast approximately 1.0-times the MRHD (10 mg/kg/day).
-
14 CLINICAL STUDIES
14.1 Psoriatic Arthritis
The safety and efficacy of OTEZLA was evaluated in 3 multicenter, randomized, double-blind, placebo-controlled trials (PsA-1 [NCT01172938], PsA-2 [NCT01212757], and PsA-3 [NCT01212770]) of similar design. A total of 1493 adult subjects with active PsA (≥ 3 swollen joints and ≥ 3 tender joints) despite prior or current treatment with disease-modifying antirheumatic drug (DMARD) therapy were randomized. Subjects enrolled in these trials had a diagnosis of PsA for at least 6 months. One qualifying psoriatic skin lesion of at least 2 cm in diameter was required in Trial PsA-3. Previous treatment with a biologic, including TNF blockers was allowed (up to 10% could be TNF blocker therapeutic failures). Across the 3 trials, subjects were randomly assigned to placebo (n = 496), OTEZLA 20 mg (n = 500), or OTEZLA 30 mg (n = 497) given orally twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Subjects were allowed to receive stable doses of concomitant methotrexate [MTX (≤25 mg/week)], sulfasalazine [SSZ (≤ 2 g/day)], leflunomide [LEF (≤20 mg/day)], low dose oral corticosteroids (equivalent to ≤10 mg of prednisone a day), and/or nonsteroidal anti-inflammatory drugs (NSAIDs) during the trial. Treatment assignments were stratified based on small molecule DMARD use at baseline in Trials PsA-1, PsA-2 and PsA-3. There was an additional stratification of body surface area (BSA) > 3% with psoriasis in Trial PsA-3. The subjects who were therapeutic failures of > 3 agents for PsA (small molecules or biologics), or > 1 biologic TNF blocker were excluded.
The primary endpoint was the percentage of subjects achieving American College of Rheumatology (ACR) 20 response at Week 16. Placebo-controlled efficacy data were collected and analyzed through Week 24. Subjects whose tender and swollen joint counts had not improved by at least 20% were considered non-responders at Week 16. Placebo non-responders were re-randomized 1:1 in a blinded fashion to either OTEZLA 20 mg twice daily or 30 mg twice daily following the titration schema [see Dosage and Administration (2.1)]. OTEZLA subjects remained on their initial treatment. At Week 24, all remaining placebo subjects were re-randomized to either 20 mg twice daily or 30 mg twice daily.
Subjects with subtypes of PsA were enrolled across the 3 trials, including symmetric polyarthritis (62.0%), asymmetric oligoarthritis (27.0%), distal interphalangeal (DIP) joint arthritis (6.0%), arthritis mutilans (3.0%), and predominant spondylitis (2.1%). The median duration of PsA disease was 5 years. Subjects received concomitant therapy with at least one DMARD (65.0%), MTX (55.0%), SSZ (9.0%), LEF (7.0%), low dose oral corticosteroids (14.0%), and NSAIDs (71.0%). Prior treatment with small-molecule DMARDs only was reported in 76.0% of subjects and prior treatment with biologic DMARDs was reported in 22.0% of subjects, which includes 9.0% who had failed prior biologic DMARD treatment.
Clinical Response in Subjects with Psoriatic Arthritis
The percent of subjects achieving ACR 20, 50 and 70 responses in Trials PsA-1, PsA-2, and PsA-3 are presented in Table 6 below. OTEZLA ± DMARDs, compared with Placebo ± DMARDs resulted in a greater improvement in signs and symptoms of psoriatic arthritis as demonstrated by the proportion of subjects with an ACR 20 response at Week 16.
Table 6: Proportion of Adult Subjects With Active Psoriatic Arthritis With ACR Responses in Trials PsA-1, PsA-2 and PsA-3 PsA-1 PsA-2 PsA-3 N* Placebo ± DMARDs
N = 168OTEZLA 30 mg twice daily ± DMARDs
N = 168Placebo ± DMARDs
N = 159OTEZLA 30 mg twice daily ± DMARDs
N = 162Placebo ± DMARDs
N = 169OTEZLA 30 mg twice daily ± DMARDs
N = 167ACR 20
Week 1619% 38% † 19% 32% † 18% 41% † ACR 50
Week 166% 16% 5% 11% 8% 15% ACR 70
Week 161% 4% 1% 1% 2% 4% OTEZLA 30 mg twice daily resulted in improvement for each ACR component, compared to placebo at Week 16 in Trial PsA-1 (Table 7). Consistent results were observed in Trials PsA-2 and PsA-3.
Table 7: ACR Components Mean Change from Baseline at Week 16 in Trial PsA-1 Placebo
(N* = 168)OTEZLA 30 mg twice daily
(N* = 168)Mean changes from baseline are least square means from analyses of covariance. - *
- N reflects randomized subjects; actual number of subjects evaluable for each endpoint may vary by timepoint.
- †
- Scale 0-78.
- ‡
- Scale 0-76.
- §
- VAS = Visual Analog Scale; 0 = best, 100 = worst.
- ¶
- HAQ-DI = Health Assessment Questionnaire – Disability Index; 0 = best, 3 = worst; measures the subject's ability to perform the following: dress/groom, arise, eat, walk, reach, grip, maintain hygiene, and maintain daily activity.
- #
- CRP = C-reactive protein; Reference range 00.5 mg/dL.
Number of tender joints† Sample Size 166 164 Baseline 23 23 Mean Change at Week 16 -2 -7 Number of swollen joints‡ Sample Size 166 164 Baseline 13 13 Mean Change at Week 16 -2 -5 Patient's assessment of pain§ Sample Size 165 159 Baseline 61 58 Mean Change at Week 16 -6 -14 Patient's global assessment of disease activity§ Sample Size 165 159 Baseline 59 56 Mean Change at Week 16 -3 -10 Physician's global assessment of disease activity§ Sample Size 158 159 Baseline 55 56 Mean Change at Week 16 -8 -19 HAQ-DI¶ score Sample Size 165 159 Baseline 1.2 1.2 Mean Change at Week 16 -0.09 -0.2 CRP# Sample Size 166 167 Baseline 1.1 0.8 Mean Change at Week 16 0.1 -0.1 Treatment with OTEZLA resulted in improvement in dactylitis and enthesitis in subjects with pre-existing dactylitis or enthesitis.
Physical Function Response
OTEZLA 30 mg twice daily demonstrated a greater improvement compared to placebo in mean change from baseline for the Health Assessment Questionnaire Disability Index (HAQDI) score at Week 16 [0.244 vs. 0.086, respectively; 95% CI for the difference was (0.26, 0.06)] in Trial PsA1. The proportions of HAQDI responders (≥ 0.3 improvement from baseline) at Week 16 for the OTEZLA 30 mg twice daily group were 38%, compared to 27%, for the placebo group in Trial PsA1. Consistent results were observed in Trials PsA2 and PsA3.
14.2 Adult Moderate to Severe Plaque Psoriasis
Two multicenter, randomized, double-blind, placebo-controlled trials (PSOR-1 [NCT01194219] and PSOR-2 [NCT01232283]) enrolled a total of 1257 subjects 18 years of age and older with moderate to severe plaque psoriasis [body surface area (BSA) involvement of ≥ 10%, static Physician Global Assessment (sPGA) of ≥ 3 (moderate or severe disease), Psoriasis Area and Severity Index (PASI) score ≥ 12, candidates for phototherapy or systemic therapy]. Subjects were allowed to use low potency topical corticosteroids on the face, axilla and groin. Subjects with plaque psoriasis of the scalp were allowed to use coal tar shampoo and/or salicylic acid scalp preparations on scalp lesions.
Trial PSOR-1 enrolled 844 subjects and Trial PSOR-2 enrolled 413 subjects. In both trials, subjects were randomized 2:1 to OTEZLA 30 mg twice daily (BID) or placebo for 16 weeks. Both trials assessed the proportion of subjects who achieved PASI-75 at Week 16 and the proportion of subjects who achieved an sPGA score of clear (0) or almost clear (1) at Week 16. Across both trials, subjects ranged in age from 18 to 83 years, with an overall median age of 46 years. The mean baseline BSA involvement was 25.2% (median 21.0%), the mean baseline PASI score was 19.1 (median 16.8), and the proportion of subjects with an sPGA score of 3 (moderate) and 4 (severe) at baseline were 70.0% and 29.8%, respectively. Approximately 30% of all subjects had received prior phototherapy and 54% had received prior conventional systemic and/or biologic therapy for the treatment of psoriasis with 37% receiving prior conventional systemic therapy and 30% receiving prior biologic therapy. Approximately one-third of subjects had not received prior phototherapy, conventional systemic nor biologic therapy. A total of 18% of subjects had a history of psoriatic arthritis.
Clinical Response in Adult Subjects with Moderate to Severe Plaque Psoriasis
The proportion of subjects who achieved PASI-75 responses, and an sPGA score of clear (0) or almost clear (1), are presented in Table 8.
Table 8: Clinical Response at Week 16 in Adults with Moderate to Severe Plaque Psoriasis in Trials PSOR-1 and PSOR-2 Trial PSOR-1 Trial PSOR-2 Placebo OTEZLA
30 mg BIDPlacebo OTEZLA
30 mg BID*N† N = 282 N = 562 N = 137 N = 274 PASI‡ -75, n (%) 15 (5.3) 186 (33.1) 8 (5.8) 79 (28.8) sPGA§ of Clear or Almost Clear, n (%) 11 (3.9) 122 (21.7) 6 (4.4) 56 (20.4) The median time to loss of PASI-75 response among the subjects re-randomized to placebo at Week 32 during the Randomized Treatment Withdrawal Phase was 5.1 weeks.
Plaque Psoriasis Involving the Scalp Area
A randomized, double-blind, placebo-controlled trial (PSOR-3 [NCT03123471]) was conducted in 303 adult subjects with moderate to severe plaque psoriasis of the scalp. Enrolled subjects had a Scalp Physician Global Assessment (ScPGA) score of ≥ 3, Scalp Surface Area (SSA) involvement of ≥ 20%, an inadequate response or intolerance to at least one topical therapy for plaque psoriasis of the scalp, and moderate to severe plaque psoriasis (BSA involvement of ≥ 10%, sPGA of ≥ 3 [moderate or severe disease], and PASI score ≥ 12).
Subjects were randomized 2:1 to receive either OTEZLA 30 mg twice daily (n =201) or placebo twice daily (n = 102) for 16 weeks. The primary endpoint was the proportion of subjects who achieved an ScPGA response at Week 16 (defined as ScPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline at Week 16). Secondary endpoints included the proportion of subjects with Whole Body Itch Numeric Rating Scale (NRS) response (defined as ≥ 4-point reduction from baseline) and the proportion of subjects with a Scalp Itch NRS response (defined as ≥ 4-point reduction from baseline).
Subjects had a mean age of 46.9 years, 61.7% were men and 75.6 % were white. At baseline, 76.9% of subjects had moderate plaque psoriasis of the scalp (ScPGA of 3), 23.1% had severe plaque psoriasis of the scalp (ScPGA of 4), 71.6% of subjects were biologic naïve, and 58.8% had failed 1 or 2 topical treatments. At baseline, the mean Whole Body Itch NRS score was 7.2 and the mean Scalp Itch NRS score was 6.7 with the scales ranging from 0 to 10. The mean baseline SSA involvement was 60.6% and the mean baseline BSA involvement was 19.8%.
The proportion of subjects who achieved an ScPGA response, Whole Body Itch NRS response, and Scalp Itch NRS response at Week 16 are presented in Table 9.
Figure 1 displays the proportion of subjects achieving Whole Body Itch NRS response at each visit, while Figure 2 displays the proportion of subjects achieving Scalp Itch NRS response at each visit.
Table 9: Efficacy Results at Week 16 in Adults with Plaque Psoriasis of the Scalp in Trial PSOR-3 Trial PSOR-3 Placebo OTEZLA
30 mg twice dailyTreatment Difference*,†
(95% CI‡)- *
- OTEZLA – Placebo.
- †
- Adjusted difference in proportions is the weighted average of the treatment differences across baseline ScPGA scores with the Cochran-Mantel-Haenszel weights.
- ‡
- CI = confidence interval.
- §
- ScPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline.
Number of subjects randomized N = 102 N = 201 ScPGA response§ 13.7% 43.3% 29.6%
(19.5%, 39.7%)Number of subjects with baseline Whole Body Itch NRS Score ≥4 N = 94 N = 185 Whole Body Itch NRS response 22.5% 45.5% 23.0%
(11.5%, 34.6%)Number of subjects with baseline Scalp Itch NRS Score ≥4 N = 90 N = 175 Scalp Itch NRS response 21.1% 47.1% 26.2%
(13.9%, 38.5%)Figure 1: Proportion (± SE) of Subjects Achieving Whole Body Itch NRS Response through Week 16 NRS = Numeric Rating Scale; SE = standard error 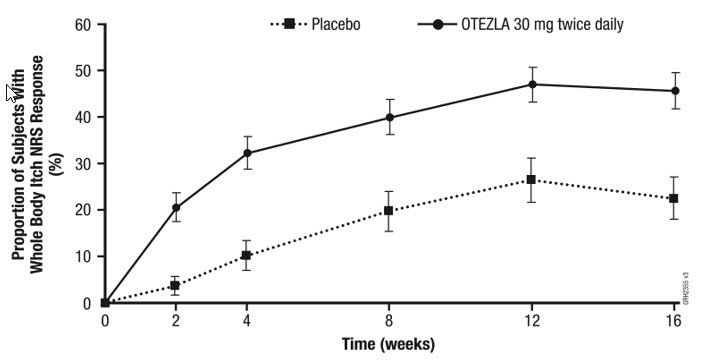
Figure 2: Proportion (± SE) of Subjects Achieving Scalp Itch NRS Response through Week 16 NRS = Numeric Rating Scale; SE = standard error 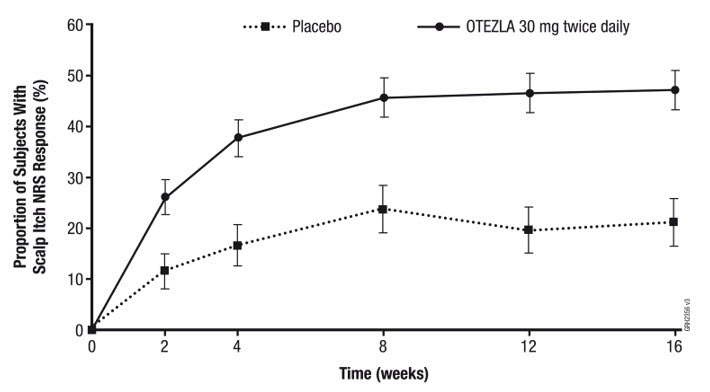
Plaque Psoriasis Involving the Genital Area
A randomized, double-blind, placebo-controlled trial (PSOR-5 [NCT03777436]) was conducted in 289 adult subjects with moderate to severe plaque psoriasis of the genital area. Subjects had a modified static Physician Global Assessment of Genitalia (sPGA-G) score of ≥ 3 (moderate or severe), sPGA score of ≥ 3 (moderate or severe), and had an inadequate response or were intolerant to topical therapy for the treatment of plaque psoriasis of the genital area.
Subjects were randomized 1:1 to receive either apremilast 30 mg twice daily (n = 143) or placebo twice daily (n = 146) for 16 weeks. At Week 16, the placebo group was switched to receive OTEZLA and the OTEZLA group remained on drug through Week 32. The primary endpoint was the proportion of subjects who achieved a modified sPGA-G response (defined as a score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16. Secondary endpoints included the proportion of subjects who achieved an sPGA response (defined as a score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16 and the proportion of subjects who achieved at least a 4-point improvement in the 11-point Genital Psoriasis Itch Numeric Rating Scale (GPI-NRS) item score within the Genital Psoriasis Symptoms Scale (GPSS) at Week 16, among subjects with a baseline GPI-NRS score of ≥ 4.
Subjects ranged in age from 18-81 years, with a median age of 44 years. The proportions of subjects with a modified sPGA-G score of 3 (moderate) and 4 (severe) at baseline were 86.9% and 13.1%, respectively. The proportions of subjects with a sPGA score of 3 (moderate) and 4 (severe) at baseline were 88.6% and 11.1%, respectively. Baseline BSA involvement was < 10% for 57.4% of the subjects and ≥ 10% for 42.6% of the subjects. The mean baseline GPI-NRS score was 6.5. Of the enrolled subjects, 78.9% did not receive prior conventional systemic therapy and 84.4% were biologic-naïve.
The proportions of subjects who achieved a modified sPGA-G response, sPGA response, and GPI-NRS response are presented in Table 10.
Table 10: Efficacy Results at Week 16 in Adults with Plaque Psoriasis of the Genital Area in Trial PSOR-5 Trial PSOR-5 Placebo OTEZLA
30 mg twice dailyTreatment Difference*,†
(95% CI)‡- *
- OTEZLA – Placebo.
- †
- Adjusted difference in proportions is the weighted average of the treatment differences across the baseline BSA strata (BSA < 10% or ≥ 10%) with the Cochran-Mantel-Haenszel weights.
- ‡
- CI = confidence interval.
- §
- Modified sPGA-G score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline. The sPGA-G scale was modified from a 6-point to a 5-point scale, ranging from 0 (clear) to 4 (severe), to assess the severity of the 3 primary signs of genital psoriasis: erythema, scaling, and plaque elevation.
- ¶
- sPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline.
- #
- GPI-NRS score reduction of ≥ 4-points from baseline.
Number of Subjects Randomized N = 146 N = 143 Modified sPGA-G Response§ 19.5% 39.6% 20.1%
(9.2%, 30.9%)sPGA Response¶ 6.9% 22.2% 15.2%
(6.9%, 23.6%)Number of Subjects with Baseline GPI-NRS Score ≥ 4 N = 121 N = 122 GPI-NRS Response# 19.6% 47.3% 27.4%
(15.4%, 39.3%)14.3 Pediatric Moderate to Severe Plaque Psoriasis
A multicenter, randomized, double-blind, placebo-controlled trial (PSOR-6 [NCT03701763]) was conducted in 245 pediatric subjects 6 to 17 years of age (inclusive) with moderate to severe plaque psoriasis who were candidates for phototherapy or systemic therapy. Subjects had an sPGA score of ≥ 3 (moderate or severe disease), BSA involvement of ≥ 10%, and PASI score of ≥ 12, with psoriasis that was inadequately controlled by or inappropriate for topical therapy. Subjects were allowed to use low potency or weak topical corticosteroids on the face, axilla, and groin and unmedicated skin moisturizers for body lesions only.
Subjects were randomized 2:1 to receive either OTEZLA (n = 163) or placebo (n = 82) for 16 weeks. Subjects with a baseline weight of 20 kg to < 50 kg received OTEZLA 20 mg twice daily or placebo twice daily, and subjects with a baseline weight ≥ 50 kg received OTEZLA 30 mg twice daily or placebo twice daily. At Week 16, the placebo group was switched to receive OTEZLA (with dosage based on baseline weight) and the OTEZLA group remained on drug (according to their original dosing assignment) through Week 52. The primary endpoint was the proportion of subjects who achieved an sPGA response (defined as a score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16. The key secondary endpoint was the proportion of subjects who achieved a PASI-75 response (at least a 75% reduction in PASI score from baseline) at Week 16.
Enrolled subjects ranged in age from 6 to 17 years, with a median age of 13 years; 41.2% of subjects were 6 to 11 years of age and 58.8% of subjects were 12 to 17 years of age. Of the enrolled subjects, 52.2% were female. For race, 86.9% were White, 3.7% were Asian, 3.3% were Black or African American, 0.8% were American Indian or Alaskan Native, and 5.3% were not reported or unknown. For ethnicity, 81.6% of subjects identified as not Hispanic or Latino, 13.1% identified as Hispanic or Latino, and 5.3% were not reported or unknown. The mean baseline BSA involvement was 31.5% (median 26.0%), the mean baseline PASI score was 19.8 (median 17.2), and the proportions of subjects with an sPGA score of 3 (moderate) and 4 (severe) at baseline were 75.5% and 24.5%, respectively. Of the enrolled subjects, 82.9% did not receive prior conventional systemic therapy and 94.3% were biologic-naïve.
Clinical Response in Pediatric Subjects 6 to 17 Years of Age and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis
The proportions of subjects who achieved sPGA response and PASI-75 response at Week 16 are presented in Table 11.
Table 11: Efficacy Results at Week 16 in Pediatric Subjects 6 to 17 Years of Age and Weighing at Least 20 kg with Moderate to Severe Plaque Psoriasis in Trial PSOR-6 Trial PSOR-6 Placebo OTEZLA* Treatment Difference†,‡
(95% CI)§- *
- Subjects weighing ≥ 50 kg received OTEZLA 30 mg twice daily and subjects weighing 20 kg to < 50 kg received OTEZLA 20 mg twice daily.
- †
- OTEZLA – Placebo.
- ‡
- Adjusted difference in proportions is the weighted average of the treatment differences across the baseline age strata (6 to 11 years of age or 12 to 17 years of age) with the Cochran-Mantel-Haenszel weights.
- §
- CI = confidence interval.
- ¶
- sPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline.
- #
- At least a 75% reduction in PASI score from baseline.
Number of Subjects Randomized N = 82 N = 163 sPGA Response¶ 10.8% 33.1% 22.3%
(12.2%, 32.4%)PASI-75 Response# 16.0% 45.7% 29.7%
(17.9%, 41.6%)14.4 Adult Mild to Moderate Plaque Psoriasis
A multicenter, randomized, double-blind, placebo-controlled trial (PSOR-4 [NCT03721172]) was conducted in 595 adult subjects with mild to moderate plaque psoriasis (BSA involvement of 2-15%, sPGA score of 2-3 [mild or moderate disease], and PASI score of 2-15). Enrolled subjects had an inadequate response or were intolerant to at least one topical therapy and had not received prior biologic therapy. Subjects were allowed to use unmedicated emollients for lesions on non-scalp areas of the body and non-medicated shampoos for lesions on the scalp.
Subjects were randomized 1:1 to receive either OTEZLA 30 mg twice daily (n = 297) or placebo twice daily (n = 298) for 16 weeks. At Week 16, the placebo group was switched to receive OTEZLA and the OTEZLA group remained on drug through Week 32. The primary endpoint was the proportion of subjects who achieved an sPGA response (defined as an sPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16. Subjects with mild disease (sPGA = 2 at baseline) were required to be clear (sPGA = 0) to achieve an sPGA response. Other evaluated endpoints include the proportion of subjects with a Whole Body Itch NRS response (defined as a ≥ 4-point reduction from baseline) at Week 16 among subjects with a baseline Whole Body Itch NRS ≥ 4 and the proportion of subjects with an ScPGA response (defined as an ScPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16 among subjects with a baseline ScPGA score ≥ 2.
Subjects ranged in age from 18 to 85 years, with an overall median age of 50 years. The mean baseline BSA involvement was 6.4%, the mean baseline PASI score was 6.5, and the proportions of subjects with an sPGA score of 2 (mild) and 3 (moderate) at baseline were 30.6% and 69.4%, respectively.
Clinical Response in Subjects with Mild to Moderate Plaque Psoriasis
The proportions of subjects who achieved an sPGA response, Whole Body Itch NRS response, and an ScPGA response at Week 16 are presented in Table 12.
Table 12: Efficacy Results at Week 16 in Adults with Mild to Moderate Plaque Psoriasis in Trial PSOR-4 Trial PSOR-4 Placebo OTEZLA
30 mg twice dailyTreatment Difference*,†
(95% CI‡)- *
- OTEZLA – Placebo.
- †
- Adjusted difference in proportions is the weighted average of the treatment differences across baseline sPGA scores with the Cochran-Mantel-Haenszel weights.
- ‡
- CI = confidence interval.
- §
- sPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline.
- ¶
- Whole Body Itch NRS score reduction of ≥ 4-points from baseline.
- #
- ScPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline.
Number of Subjects Randomized N = 298 N = 297 sPGA Response§ 4.1% 21.6% 17.5%
(12.2%, 22.8%)Number of Subjects with Baseline Whole Body Itch NRS Score ≥ 4 N = 249 N = 253 Whole Body Itch NRS Response¶ 18.6% 43.2% 24.7%
(16.5%, 32.8%)Number of Subjects with Baseline ScPGA Score ≥ 2 N = 199 N = 212 ScPGA Response# 16.6% 44.0% 27.4%
(18.6%, 36.3%)14.5 Oral Ulcers Associated with Behçet's Disease
A multicenter, randomized, placebo-controlled trial (BCT-002 [NCT02307513]) enrolled a total of 207 adult subjects with BD with active oral ulcers. Subjects were previously treated with at least one nonbiologic BD medication and were candidates for systemic therapy. Subjects met the International Study Group (ISG) Criteria for BD. Subjects had at least 2 oral ulcers at screening and at least 2 oral ulcers at randomization and without currently active major organ involvement. Concomitant treatment for BD was not allowed.
Subjects were randomized 1:1 to receive either OTEZLA 30 mg twice daily (n = 104) or placebo (n = 103) for 12 weeks. After Week 12, all subjects received OTEZLA 30 mg twice daily.
Efficacy was assessed based on the number and pain of oral ulcers.
Subjects ranged in age from 19 to 72 years, with a mean age of 40 years. The mean duration of BD was 6.84 years. All subjects had a history of recurrent oral ulcers that were currently active. Subjects had a history of skin lesions (98.6%), genital ulcers (90.3%), musculoskeletal manifestations (72.5%), ocular manifestations (17.4%), central nervous system (9.7%), gastrointestinal (GI) manifestations (9.2%) and vascular involvement (1.4%). The mean baseline oral ulcer counts were 4.2 and 3.9 in the OTEZLA and placebo groups, respectively.
Measures of Oral Ulcers
Improvements in measures of oral ulcers at Week 12 are presented in Table 13.
Table 13: Clinical Response of Oral Ulcers at Week 12 in Adult Subjects with BD in the BCT-002 Trial (ITT* Population) Endpoint Placebo
N = 103OTEZLA
30 mg twice daily
N = 104Treatment Difference†
(95% CI‡)- *
- ITT = intent to treat.
- †
- OTEZLA – Placebo.
- ‡
- CI = confidence interval.
- §
- Mean changes from baseline are least square means from mixed effects- model for repeated measures, adjusting for sex, region, and baseline pain of oral ulcers as measured by the visual analog scale.
- ¶
- VAS = visual analog scale; 0 = no pain, 100 = worst possible pain.
- #
- Subjects for whom data are not available to determine response status are considered non-responders-.
- Þ
- Adjusted difference in proportions is the weighted average of the treatment differences across the 4 strata of combined sex and region factors with the Cochran-Mantel-Haenszel weights.
- ß
- Mean daily averages are least squares means from analysis of covariance, after adjusting for sex, region, and baseline number of oral ulcers.
- à
- Based on oral ulcer counts measured at baseline and at Weeks 1, 2, 4, 6, 8, 10, and 12.
Change§ from baseline in the pain of oral ulcers as measured by VAS¶ at Week 12 −18.7 −42.7 −24.1
(−32.4, −15.7)Proportion# of subjects achieving oral ulcer complete response (oral ulcer-free) at Week 12 22.3% 52.9% 30.6%Þ
(18.1%, 43.1%)Proportion# of subjects achieving oral ulcer complete response (oral ulcer -free) by Week 6, and who remained oral ulcer -free for at least 6 additional weeks during the 12-week Placebo-controlled Treatment Phase 4.9% 29.8% 25.1%#
(15.5%, 34.6%)Daily averageß,à number of oral ulcers during the 12-week Placebo-controlled Treatment Phase 2.6 1.5 −1.1
(−1.6, −0.7)Figure 3 displays the mean number of oral ulcers for each treatment group at each visit, while Figure 4 displays the mean oral ulcer pain on a visual analog scale for each treatment group at each visit.
Figure 3: Mean (± SE) Number of Oral Ulcers by Time Point Through Week 12 (ITT Population) 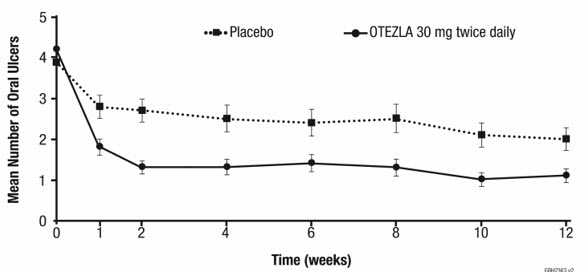
Weeks 0 1 2 4 6 8 10 12 ITT = intent-to-treat; SE = standard error Placebo, n 103 98 97 93 91 86 83 82 OTEZLA 30 mg twice daily, n 104 101 101 101 98 94 94 97 Figure 4: Mean (± SE) Oral Ulcer Pain on a Visual Analog Scale by Time Point Through Week 12 (ITT Population) 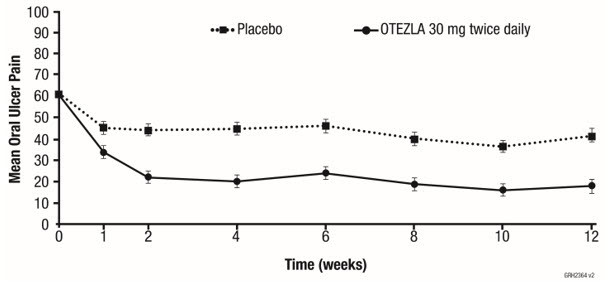
Weeks 0 1 2 4 6 8 10 12 ITT = intent to treat; SE = standard error.
Oral ulcer pain was assessed on a 100-mm Visual Analog Scale with 0 = no pain and 100 = worst possible pain. Mean baseline Visual Analog Scale pain scores were 61.2 and 60.8 in the OTEZLA 30 mg twice daily treatment group and placebo treatment group, respectively.Placebo, n 101 95 96 91 90 85 82 81 OTEZLA 30 mg twice daily, n 102 95 97 99 97 92 93 95 -
16 HOW SUPPLIED/STORAGE AND HANDLING
OTEZLA is available as diamond-shaped, film-coated tablets in the following dosage strengths: 10 mg pink tablet engraved with "APR" on one side and "10" on the other side; 20 mg brown tablet engraved with "APR" on one side and "20" on the other side; 30 mg beige tablet engraved with "APR" on one side and "30" on the other side.
Tablets are supplied in the strengths and package configurations listed in Table 14.
Table 14: OTEZLA Package Configurations Package configuration Tablet strength NDC number Configurations for 30 mg BID Dosage 28-day treatment initiation pack 55-tablet blister pack including tablets for titration and maintenance dosage: 4 tablets (10 mg each), 4 tablets (20 mg each), and 47 tablets (30 mg each) 55513-369-55 60-count bottle 30 mg 55513-137-60 Configurations for 20 mg BID Dosage 28-day treatment initiation pack 55-tablet blister pack including tablets for titration and maintenance dosage: 4 tablets (10 mg each) and 51 tablets (20 mg each) 55513-508-55 60-count bottle 20 mg 55513-497-60 -
17 PATIENT COUNSELING INFORMATION
• Administration Instructions
Instruct patients to take OTEZLA only as prescribed [see Dosage and Administration (2.1 and 2.2)].
Advise patients to take OTEZLA with or without food. Instruct patients to swallow tablets whole and not to crush, split, or chew prior to swallowing [see Dosage and Administration (2.3)].
• Hypersensitivity
Inform patients that hypersensitivity reactions can occur following administration of OTEZLA. Instruct patients to contact their healthcare provider if they experience symptoms of an allergic reaction [see Warnings and Precautions (5.1)].
• Diarrhea, Nausea, and Vomiting
Advise patients of the potential complications of severe diarrhea, nausea, or vomiting and instruct them to contact their healthcare provider if they experience these adverse reactions, especially if the patient is 65 years of age or older [see Warnings and Precautions (5.2)].
• Depression
Inform patients that treatment with OTEZLA is associated with an increased incidence of depression. Advise patients, their caregivers, and families of the need to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes, and if such changes occur to contact their healthcare provider [see Warnings and Precautions (5.3)].
• Weight Decrease
Inform patients that treatment with OTEZLA is associated with potential weight loss. Instruct patients or caregivers to have their or their child's weight monitored regularly and, if unexplained or clinically significant weight loss occurs, to contact their healthcare provider for evaluation of the weight loss [see Warnings and Precautions (5.4)].
• Pregnancy
Advise pregnant patients and patients of reproductive potential of the potential risk to a fetus. Advise patients to inform their prescriber of a known or suspected pregnancy [see Use in Specific Populations (8.1)].
- SPL UNCLASSIFIED SECTION
- PRINCIPAL DISPLAY PANEL - 60 Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 28 Day Treatment Initiation Pack
-
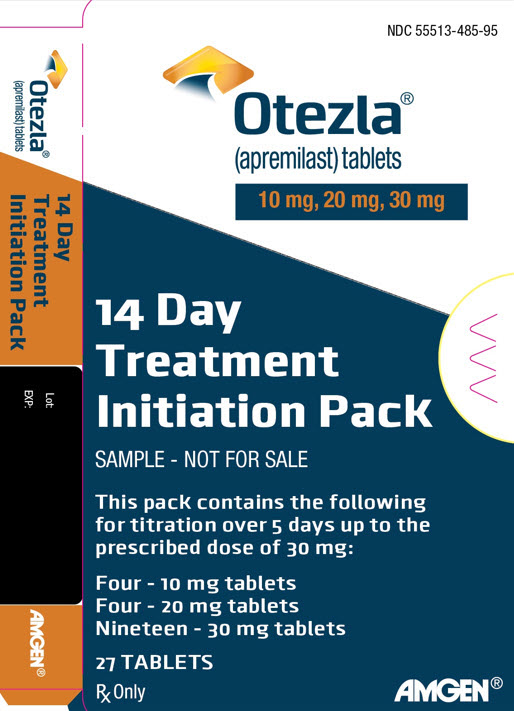
PRINCIPAL DISPLAY PANEL - 14 Day Treatment Initiation Pack - 55513-485-95
NDC 55513-485-95
Otezla®
(apremilast) tablets
10 mg, 20 mg, 30 mg14 Day
Treatment
Initiation PackSAMPLE - NOT FOR SALE
This pack contains the following
for titration over 5 days up to the
prescribed dose of 30 mg:Four - 10 mg tablets
Four - 20 mg tablets
Nineteen - 30 mg tablets27 TABLETS
Rx Only
AMGEN®
-
PRINCIPAL DISPLAY PANEL - 14 Day Treatment Initiation Pack - 55513-485-96
NDC 55513-485-96
14 Day Treatment
Initiation PackSAMPLE - NOT FOR SALE
Each pack contains the following for titration
over 5 days up to the prescribed dose of 30 mg:
Four - 10 mg tablets
Four - 20 mg tablets
Nineteen - 30 mg tablets
Five starter packs each containing 27 TABLETSRx Only
AMGEN®
Otezla®
(apremilast) tablets
- PRINCIPAL DISPLAY PANEL - 60 Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 28 Day Treatment Initiation Pack - 55513-508-55
-
PRINCIPAL DISPLAY PANEL - 14 Day Treatment Initiation Pack - 55513-996-95
NDC 55513-996-95
14 Day Treatment
Initiation PackSAMPLE - NOT FOR SALE
Each pack contains the following for titration over
3 days up to the prescribed dose of 20 mg:
Four - 10 mg tablets
Twenty-three - 20 mg tablets
Three starter packs each containing 27 TABLETSRx Only
AMGEN®
Otezla®
(apremilast) tablets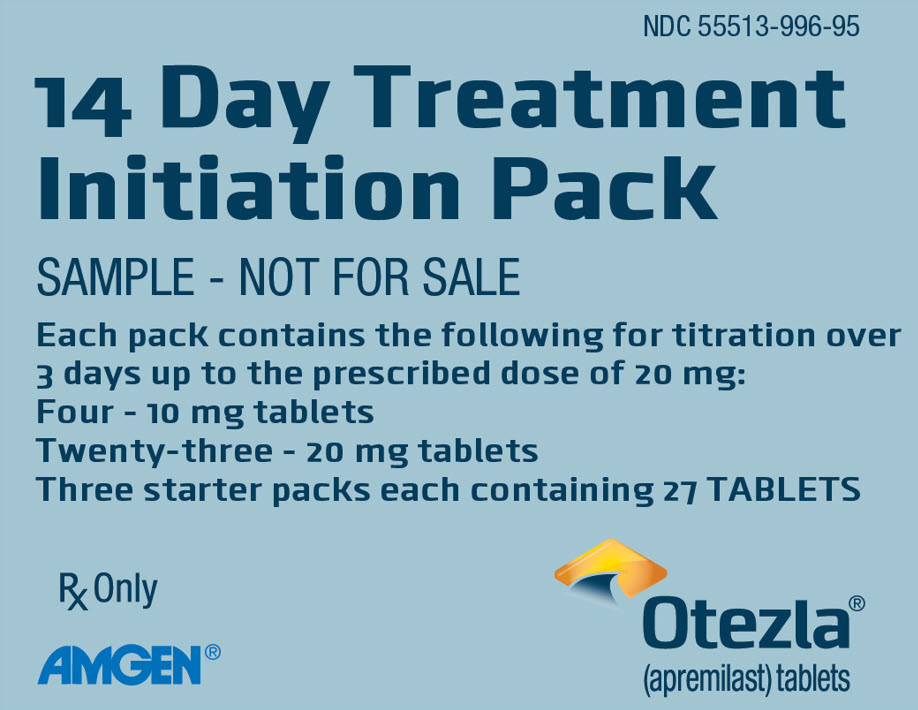
- PRINCIPAL DISPLAY PANEL - 14 Day Treatment Initiation Pack - 55513-996-96
-
INGREDIENTS AND APPEARANCE
OTEZLA
apremilast tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55513-137 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 30 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color WHITE (Beige) Score no score Shape DIAMOND Size 12mm Flavor Imprint Code APR;30 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-137-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 02/26/2020 2 NDC:55513-137-95 1 in 1 CARTON 02/26/2020 2 28 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 OTEZLA
apremilast kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55513-369 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-369-55 1 in 1 CARTON 02/26/2020 1 1 in 1 BLISTER PACK Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 4 Part 2 4 Part 3 47 Part 1 of 3 OTEZLA
apremilast tablet, film coatedProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 10 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color PINK Score no score Shape DIAMOND Size 8mm Flavor Imprint Code APR;10 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 Part 2 of 3 OTEZLA
apremilast tablet, film coatedProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 20 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BROWN Score no score Shape DIAMOND Size 10mm Flavor Imprint Code APR;20 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 Part 3 of 3 OTEZLA
apremilast tablet, film coatedProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 30 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color WHITE (Beige) Score no score Shape DIAMOND Size 12mm Flavor Imprint Code APR;30 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 OTEZLA
apremilast kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55513-485 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-485-96 5 in 1 CARTON 02/26/2020 1 NDC:55513-485-95 1 in 1 BLISTER PACK Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 4 Part 2 4 Part 3 19 Part 1 of 3 OTEZLA
apremilast tablet, film coatedProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 10 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color PINK Score no score Shape DIAMOND Size 8mm Flavor Imprint Code APR;10 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 Part 2 of 3 OTEZLA
apremilast tablet, film coatedProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 20 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BROWN Score no score Shape DIAMOND Size 10mm Flavor Imprint Code APR;20 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 Part 3 of 3 OTEZLA
apremilast tablet, film coatedProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 30 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color WHITE (Beige) Score no score Shape DIAMOND Size 12mm Flavor Imprint Code APR;30 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 02/26/2020 OTEZLA
apremilast tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55513-497 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 20 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BROWN (Brown) Score no score Shape DIAMOND Size 10mm Flavor Imprint Code APR;20 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-497-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 04/27/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 OTEZLA
apremilast kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55513-508 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-508-55 1 in 1 BLISTER PACK 04/27/2024 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 BLISTER PACK 4 Part 2 1 BLISTER PACK 51 Part 1 of 2 OTEZLA
apremilast tablet, film coatedProduct Information Item Code (Source) NDC:55513-518 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 10 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color PINK Score no score Shape DIAMOND Size 8mm Flavor Imprint Code APR;10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-518-04 4 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 Part 2 of 2 OTEZLA
apremilast tablet, film coatedProduct Information Item Code (Source) NDC:55513-497 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 20 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BROWN (Brown) Score no score Shape DIAMOND Size 10mm Flavor Imprint Code APR;20 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-497-51 51 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 OTEZLA
apremilast kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55513-996 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-996-95 3 in 1 CARTON 04/27/2024 1 NDC:55513-996-96 1 in 1 BLISTER PACK Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 BLISTER PACK 4 Part 2 1 BLISTER PACK 23 Part 1 of 2 OTEZLA
apremilast tablet, film coatedProduct Information Item Code (Source) NDC:55513-518 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 10 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color PINK Score no score Shape DIAMOND Size 8mm Flavor Imprint Code APR;10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-518-04 4 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 Part 2 of 2 OTEZLA
apremilast tablet, film coatedProduct Information Item Code (Source) NDC:55513-497 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength APREMILAST (UNII: UP7QBP99PN) (APREMILAST - UNII:UP7QBP99PN) APREMILAST 20 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BROWN (Brown) Score no score Shape DIAMOND Size 10mm Flavor Imprint Code APR;20 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55513-497-23 23 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA205437 04/27/2024 Labeler - Amgen Inc (039976196) Registrant - Amgen, Inc (039976196)